A muscle relaxant, also known as spasmolytic, is a medication that patients use to relieve short-term musculoskeletal pains. OTC muscle relaxers are used for the treatment of acute pain and prescription muscle relaxers are used to manage chronic pain that lasts longer than 3 months. For patients taking muscle relaxers with alcohol, it is important to ask the question: can you drink on muscle relaxers? Remember that alcohol is contraindicated for many types of medications.
Table Of Contents:
In 2011, it was reported that 18% of 50,000 hospital visits due to muscle relaxer abuse involve alcohol use. Muscle relaxers and alcohol side effects are similar. Both muscle relaxants and alcohol deliver a depressant effect and act on the central nervous system. This causes the body functions to slow down, which includes the heartbeat and breathing. In essence, drinking alcohol usually interacts with one or more components in medications and causes its impact on the body to become magnified, making muscle relaxers overdose highly likely. In this article, information about muscle relaxer side effects, how to manage muscle relaxant interactions, and how to avoid muscle relaxers addiction and abuse will be provided.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
More About Muscle Relaxants:
Can You Drink On Muscle Relaxers?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) states that mixing alcohol and medicine, which includes mixing spasmolytic drugs and beer, may interact in dangerous ways even when these are not taken together. The agency also notes two other factors that may increase risks for muscle relaxants and alcohol interactions such as sex and age, and women and older people are more susceptible to the side effects of combining muscle relaxers with alcohol.
Generally, it is not safe for health to drink while on these medications. In one case from Pittsburgh Criminalistics Laboratory, it was reported that one patient died due to drowning after drinking alcohol with an antispasmodic medication named Cyclobenzaprine. In this case, the reason behind the fatal health event was because of the severe sedation experienced by the patient. Although the many uses of muscle relaxers help in improving the daily lives of patients, users of these drugs should know their dangers as well.
Muscle Relaxers And Alcohol Side Effects
Combining alcohol and muscle relaxers intensifies the sedating effects of both substances. On that note, how long does it take for muscle relaxers to kick in? Most of these drugs begin affecting the system within 30 minutes from intake and stay in effect for as long as six hours. During this time, side effects associated with these drugs also become noticeable and may become gravely magnified with drinking liquor.
These centrally acting muscle relaxants can produce dangerous side effects and this is why other measures, such as the use of herbal or natural muscle relaxants or taking non-steroidal anti-inflammatory drugs (NSAID), must first be explored before taking prescription-only spasmolytic drugs. In this section, side effects that may arise from alcohol-muscle relaxant interactions will be discussed.
Nervous System Side Effects of Alcohol and Muscle Relaxers
Combining muscle relaxers and alcohol increases adverse impacts on the nervous system, which include difficulty concentrating, impaired motor skills, sleepiness, and dizziness. As cited by medical professors from Indiana, this interaction of muscle relaxants and alcohol mostly occurs in the central nervous system. Generally, alcohol alters the effects of the medication without affecting the concentration of the drug in the blood.
Based on pharmacologists from Tennessee, with increasing dependence, misuse, or abuse, these side effects, including impaired thinking, confusion, memory lapses, and poor judgment, become more frequent and impact on the nervous system becomes more permanent.
Digestive Issues
These drugs are completely absorbed by the gastrointestinal tract, and in one report from Tulane University, common complaints related to this body part include constipation, dyspepsia, nausea, emesis, metallic taste, and dry mouth. Overtime or with increasing dependence, this can lead to cholestatic jaundice, liver damage, kidney damage, and edema. On the other hand, an alcoholic drink can cause gastritis. Eventually, the combination of alcohol with muscle relaxers can make gastritis become a long-lasting condition.
Poor Coordination
Combining muscle relaxers and alcohol also makes motor control and coordination more difficult as a result of severe sedation. In a report published in the Journal of Forensic Sciences, poor coordination can cause driving impairment and the reported driving behaviors include erratic lane travel, slow driving, repeated swerving, stopping in traffic, and hitting parked cars and stationary objects. For these reasons, it is vital not to drive or operate machinery when one is taking these spasmolytic drugs, and of course, if these drugs are mixed with an alcoholic drink.
Poor Vision
Poor vision is a rare side effect of these drugs. However, people who abuse muscle relaxers and alcohol commonly experience blurred vision. In a study of pharmacists from Missouri, the odds ratio of patients experiencing poor vision after taking alcohol with muscle relaxers is 2.09. Over time, this can lead to permanent damage to the eyes. Having said this, it is highly recommended for those mixed muscle relaxers and alcohol together to avoid operating machinery as this can lead to fatal accidents.
Increased Risk For Addiction And Overdose
Muscle relaxants, especially benzodiazepines, are addictive substances. This goes the same for alcohol. When these two are mixed, the risk of addiction can be increased. Early signs of addiction to this drug-alcohol combination such as slow or shallow breathing and slower heartbeat may lead to chronic fainting, low blood pressure, higher risk for experiencing seizures, and death.
In which case, prompt detoxification as part of a more comprehensive professional medical treatment comes highly recommended to prevent dangerous side effects from escalating to irreversible and more severe complications.

What To Do If One Has Already Had Alcohol?
Some users of these drugs may not be aware that it is dangerous to mix these drugs with an alcoholic drink. Thus, patients should know how to manage this interaction.
In case a spasmolytic medication and alcohol have been taken together, follow the tips below to help ensure one’s safety:
- Ask for help. This interaction of alcohol and muscle relaxers will make one dizzy and impair the focus. It is essential to be with someone a patient trusts during this time.
- Note signs and symptoms of overdose. Other than the side effects mentioned above, look out for the following: excessive sweating, hallucinations, and violent behavior.
- Administer first aid as needed. Check for pulse and open up the airways. Ask for medical emergency help. While waiting for the emergency team to arrive, try to get more information on what specific drugs and an alcoholic drink was taken, and how much time has elapsed since intake.
Take note that intense sedation and severe side effects like respiratory depression are results of overdose due to this interaction of alcohol and muscle relaxers. In case any of these signs and symptoms appear, it is highly advised to call the nearest poison center or 911 to avoid further unwanted health events.
When Is It Safe To Drink Again?
Keep in mind that alcohol and muscle relaxers should not be taken at the same time. This interaction can potentially endanger one’s health and safety. If possible, patients should avoid drinking an alcoholic drink as long as they are on antispasmodic medication therapy. Generally, the half-life of alcohol is around 5 hours. On the other hand, some spasmolytic medications, like the drug Flexeril, take up to more than one week before they are completely cleared from the system. This makes consulting with the doctor imperative so that the half-life of the specific muscle relaxant taken can be established. Besides, different medications interact with alcohol differently.
In the case of misusing muscle relaxers with alcohol, the person affected and his or her loved ones should consider enrollment in a rehab program that includes the supervision of a medical professional to improve the prospect of sustainable recovery.
Always Seek The Advice of a Doctor
Indeed, muscle relaxers are effective medications for the management and treatment of acute to chronic pain. Since these drugs are also available as OTC medications, those taking them should know that there are interactions that should be avoided, and one of these includes the use of alcohol. Mixing alcohol and muscle relaxers can increase sedation which can lead to fatality.
Aside from this, addiction to both substances can also arise from mixing alcohol with muscle relaxers. Patients who are struggling with alcohol addiction can consider joining Alcoholics Anonymous meetings. At rehab centers, there is also a 12-Step Program and Technique to ensure patients a successful recovery. Healthcare professionals in these institutions can also provide tips to patients on how to detoxify from an alcoholic drink at home.
Furthermore, those who are addicted to muscle relaxers can consider drug addiction treatment at in-patient rehab centers or outpatient rehab centers. At these resources, a drug intervention program can be given by an addiction specialist and a relapse prevention plan can be formulated for a more successful recovery. Even during this time of the Covid-19 pandemic, addiction treatment is possible.
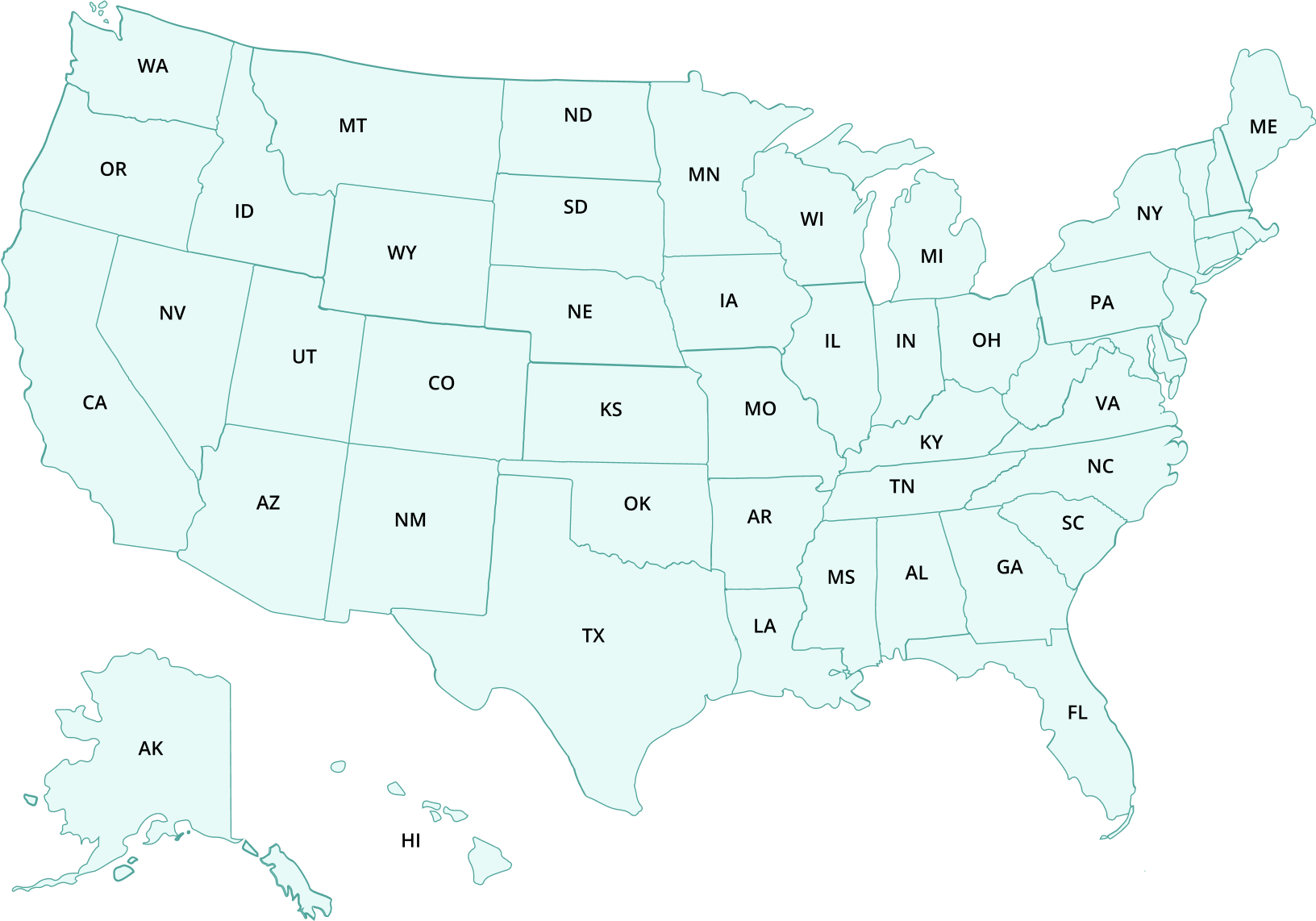
Find Drug Rehabilitation Centers Near You Anywhere In the US
Addiction Resource team has compiled an extensive list of the top drug rehabilitation facilities around the country. Click on the state you are interested in, and you'll get a list of the best centers in the area, along with their levels of care, working hours, and contact information. Haven't found the rehab you need? Call the toll-free helpline below for professional assistance.
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- West Virginia
- Wisconsin
- Wyoming
Page Sources
- Ball, J. K., & Albright, V. (2008). Drug Abuse Warning Network, 2006: national estimates of drug-related emergency department visits. Annotation.
- Ferslew, K. E., Hagardorn, A. N., & McCormick, W. F. (1990). A fatal interaction of methocarbamol and ethanol in an accidental poisoning. Journal of Forensic Science, 35(2), 477-482.
- Hetland, A., & Carr, D. B. (2014). Medications and impaired driving. Annals of pharmacotherapy, 48(4), 494-506.
- Jones, A. W. (1987). Elimination half‐life of methanol during hangover. Pharmacology & toxicology, 60(3), 217-220.
- Logan, B. K., Case, G. A., & Gordon, A. M. (2000). Carisoprodol, meprobamate, and driving impairment. Journal of Forensic Science, 45(3), 619-623.
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2021, December 15). National Institutes of Health (NIH). https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-institute-alcohol-abuse-alcoholism-niaaa
- Weathermon, R., & Crabb, D. W. (1999). Alcohol and medication interactions. Alcohol Research & Health, 23(1), 40.
- Winek Jr, C. L., Wahba, W. W., & Winek, C. L. (1999). Drowning due to cyclobenzaprine and ethanol. Forensic science international, 100(1-2), 105-108.

 Authored by
Authored by  Reviewed by
Reviewed by 


