Patients treated for substance use disorder often fall back to their old addictive habits, which becomes a source of frustration for them and their families. Many think a lapse means the failure of a patient to recover successfully. They’re mistaken. Many factors may contribute to a drug relapse.
Table Of Contents:
Some common causes of drug relapse include stress, continued exposure to people or places connected to addictive behavior, and negative emotions. Being near the object of your addiction, such as alcohol, can lead to an alcohol relapse and even happy moments like celebrations where the substance of addiction is served, such as alcohol-containing cocktails.
What is a relapse? What causes it? And, finally, how to set up a relapse prevention plan?
What Is a Relapse?
Drug abuse is a long-term condition similar to other chronic diseases, and therefore relapses are a common complication on the road to recovery. What is a relapse? It occurs when a former drug abuser returns to drug use after prolonged sobriety, such as methamphetamine, opioid, alcohol relapse, and so on. It may be a full relapse or a “slip.”
Certain evidence has shown that up to two-thirds of chronic drug users slip up within weeks to months of starting treatment, and up to 85 percent of users return to drug use within one year of quitting. These statistics can help you process just how common drug relapse is and how drug addiction is a chronic but curable condition that requires prolonged treatment, just like any other chronic disorder.
The stages of change model is often used to help explain why people suffering from substance use disorder typically undergo a recidivism cycle before quitting for good. According to this model, people do not change addictive behavior following a unidirectional route. Proponents of this model define a lapse as a process, cycling through different stages that may be interrupted by recidivism from time to time.
Causes Of Addicts Relapse
According to NIDA, addiction recidivism is a normal part of recovery. However, although recidivism is part of recovery, the NIDA cautions that it can be extremely dangerous, sometimes even deadly with some drugs. For the NIDA, relapse means the same way as when it occurs in other chronic medical illnesses. Drug relapse in addiction can result from triggers, ceasing medical treatment, or incompatible medications and treatment programs.

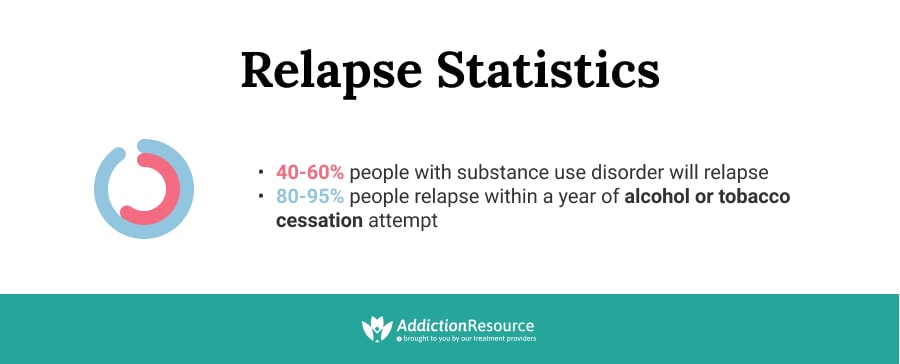
In a study published in the Journal of the American Medical Association, relapsing in substance use disorders was compared to relapsing among those suffering from hypertension and asthma. Study results showed that 40% to 60% of recovering addicts suffer from it at least once, whereas worsening occurs in 50% to 70% of people with health conditions such as hypertension and asthma.
Preventing the worsening is a critical part of all drug treatment programs and involves identifying the warning signs and triggers. By improving awareness of the people, places, things, feelings, events that can catalyze drug cravings, the patient can better devise alternatives on how to identify the triggers, get help immediately, and determine when he is about to slip up. Family and friends are encouraged to educate themselves on how to stop enabling an addict and help them stay clean.
The Stages Of Drug Relapse
While experts agree that recidivism is part of recovery and happens gradually, there are different explanations of its phases and warning signs.
There Are Three Main Stages of Drug Relapse:
- Phase 1: Emotional. This phase is highlighted by poor self-care, destructive behavior, and emotional triggers. Common emotional triggers include hunger, anger, poor health, loneliness, reduced contact with friends and family, and tiredness. Anger management and mind-body relaxation techniques to teach the patient how to better cope with negative emotions.
- Phase 2: Mental. This phase can happen after or simultaneously with the emotional phase. This next phase is the bargaining stage, where the patient is continuously weighing the pros and cons of using or drinking.
- Phase 3: Physical. The last of the recidivism phases and warning signs is the stage when a patient starts using again.
How To Create a Relapse Prevention Plan
First, recovering addicts must acknowledge that relapse is always possible. By recognizing this reality, patients should be motivated to stay on guard and learn as much as they can about how to prevent it. Patients should be able to identify red flags in their behavior and emotional and mental states. If red flags can be spotted early on, the patient can roll out mitigating measures to stop progression to recidivism as soon as possible.
One of the best ways to do this is by following a technique called the relapse prevention plan. What is it? A relapse prevention plan is a system that outlines the steps the recovering drug abuser will take to avoid recidivism and the measures to be taken if recidivism does occur. This is an effective way to avoid contact with potential triggers and avoid spiraling back into full recidivism in the event of a slip-up. This plan should be written down and reviewed regularly as one passes through the various stages of recovery. This process may be done by yourself or with professional assistance.
Make a Reminder of Warning Signs
One vital component of the relapse prevention plan is looking out for and avoiding contact with potential triggers during treatment. If one has already relapsed in the past, it is essential to write down the list of triggers that led to recidivism. Also, a list of personalized and generalized warning signs before a potential slip-up is helpful. This may include things such as how one felt before relapsing, activities, warning signs such as increasing isolation, mood swings, a decline in self-care, developing cross addictions, and so on.

It will give a warning and help preempt another potential slip-up and give an addict ample time to follow the relapse prevention plan when the early warning signs occur.
Remember the Reason For Quitting
Another essential thing to keep in mind is the reason one decided to quit in the first place. It can serve as a source of inspiration and help strengthen one’s resolve when it’s weakening. In addition, it can be helpful to weigh the pros and cons of quitting and even write them down as a part of the relapse prevention plan to regularly reinforce the decision. Patients are encouraged to review this list when they need motivation or experience triggers.
It Can Be Done as Follows:
- In one column, patients list down what they love about addiction, what benefits they get from it, and what they hate about giving it up.
- In another column, patients list down what they hate about addiction and what good things they suppose will happen if they give it up.
Set Goals
Set recovery goals. For this recidivism prevention activity to become more worthwhile, therapists recommend breaking down goals into smaller bits and pieces that can be achieved over shorter periods.
A relapse prevention plan worksheet that starts with setting personal goals for wanting to stay sober helps a patient find a life purpose. It keeps the patient’s mind distracted and away from the object of addiction.
It May Consist Of:
- Skills and career development
- Repairing broken relationships
- Pursuing hobbies that restore mental and physical health
- Growing spiritually
List Your Triggers and Coping Strategies
Recidivism triggers are external or internal cues that cause a person in addiction recovery to crave drugs and may eventually lead to a slip-up. These may vary widely from person to person, and therefore it is helpful to write down your triggers and other things that reminded you of past drug abuse. Some common triggers include people, places, or things associated with the substance of abuse, situations such as celebrations, social gatherings, negative emotions, boredom, and even positive emotions like excitement and passion.
Common Triggers Can Be Grouped Into Five Categories:
- Physical
- Emotional
- Psychological
- Social
- Environmental
By knowing the triggers, the patient can put mitigation measures in place. That’s where getting help and pursuing personal development come into play, to help counter them.
Coping Strategies
Another important part of your recidivism prevention plan is what to do when faced with potential triggers. Take care to clearly outline and write this down in your recidivism prevention plan. It may include moving to a different district or town of your immediate vicinity that reminds you of drug abuse, picking up stress-relieving practices like yoga or sports, and even therapy and counseling.
Know Where to Get Help
Remember that recidivism is a widespread complication encountered on the road to recovery and sometimes may feel closer than usual due to various factors. Therefore, it is important to have a list of close people you can contact for help during times like these. Counseling or 12-step programs can also be an important source of support for individuals struggling with recovery from drug abuse and the health complications associated with the condition. Some popular counseling programs include Alcoholics Anonymous for those struggling with alcohol relapse, Celebrate Recovery, Cocaine Anonymous, and so on. Friends, family, and even religious organizations are also important support groups for struggling addicts.
Identify Actions to Take When Relapse Occurs
Since the possibility for deterioration is high, recidivism prevention worksheets also include activities where the individual must lay out a plan in case the worst does happen. Some common options may include reaching out for help immediately, attending self-help groups, avoiding further contact with potential triggers such as alcohol and illicit drugs.
Relapse Prevention Planning Worksheet
A relapse prevention planning worksheet can be helpful for those who find it difficult to write it themselves. A relapse prevention planning worksheet gives you a basic outline of what a good prevention process looks like and allows you to personalize it further to fit your unique needs and aid you during the recovery process.

Relapse Prevention Models
A relapse prevention model is a simplistic way of explaining what motivates a person to stay sober and what factors contribute to a slip-up. By understanding what drives it, mitigating measures may be put in place to increase the patient’s chances of full recovery.
Three Prevention Models Are Described Below:
Marlatt Relapse Prevention Model
This model is based on three significant thrusts that helped shape prevention practices today:
- A patient must believe in their capacity to stay sober.
- A patient must value the tangible and intangible benefits of giving up addiction.
- A patient must gain the power to control their internal and external triggers to catalyze positive behavior change.
A substance abuse worksheet will typically include activities centered on improving the patient’s self-efficacy to continue abstinence and stay goal-driven, both of which can decrease the probability of lapse according to this paradigm.
Gorski Relapse Prevention Model
Identifying triggers, applying measures to mitigate triggers, planning for recovery, daily scheduling, and family involvement are all critical components of recidivism prevention approaches to treatment anchored on the Gorski relapse prevention model.
There Are Nine Basic Principles in the Gorsky Prevention Model:
- Self-regulation. It involves completing treatment and detaching oneself from drug use and triggers.
- Principle of Integration. Resolving past issues driving addiction.
- Principle of Understanding. The patient and his loved ones are well-informed about the real and continuing possibility of relapse, stages, and triggers.
- Self-knowledge. It involves identifying triggers, including drivers of past lapses and root causes of addiction, such as family problems and a history of substance abuse.
- Coping Skills. The Gorski prevention model emphasizes on improving individual efficacy to prevent and respond to triggers.
- Recovery Planning. Addiction recovery worksheets help the patient come up with a prevention plan.
- Inventory Training. It involves daily scheduling to avoid triggers.
- Involvement of significant others. A patient requires an active personal support group to deal with recovery challenges and the high likelihood of a slip-up.
- Maintenance and follow-up. Gorski stresses that for addiction recidivism prevention to become effective. It involves finding the right balance of programs and activities that increases a patient's chances of full recovery.
Melemis Relapse Prevention Plan
This plan proposes five rules for a patient to live by – five recidivism prevention tips, which should significantly decrease the likelihood of relapse.
The Five Rules Are:
- Rule 1: Change a life. A personal prevention plan must not only include drastic changes to avoid triggers but also incorporate new routines, hobbies, interests, people, and environments in patients' lives. These things make it easier for them to stay free of addiction.
- Rule 2: Be completely honest. Melemis writes, "Addiction requires lying." The proponent recommends setting up recovery circles that involve a patient's support group and where all members are completely honest with each other.
- Rule 3: Ask for help. Participation in self-help groups gives patients a better perception that they are not alone going through the tough challenges associated with recovery. The participation also shows them that others can do it and reminds them about the consequences.
- Rule 4: Practice self-care. Patients must find healthier alternatives to have fun and relax.
- Rule 5: Don't bend the rules. The patient must learn to abide by the rules at all times and not make excuses to justify non-adherence.
Prevent Relapse Successfully
Improving the patient’s self-efficacy to resist addiction triggers and create a new life free from substance dependence is possible. The reality, however, remains: the possibility of a lapse is high.
By working through this recidivism prevention plan example, patients can deal more effectively with their triggers and cravings and stay on track to fully recover from addiction. While patients may be strong-willed and highly motivated to maintain sobriety, they will need all of the help to overcome addiction, from both personal and professional circles.
Find Drug Rehabilitation Centers Near You Anywhere In the US
Addiction Resource team has compiled an extensive list of the top drug rehabilitation facilities around the country. Click on the state you are interested in, and you'll get a list of the best centers in the area, along with their levels of care, working hours, and contact information. Haven't found the rehab you need? Call the toll-free helpline below for professional assistance.
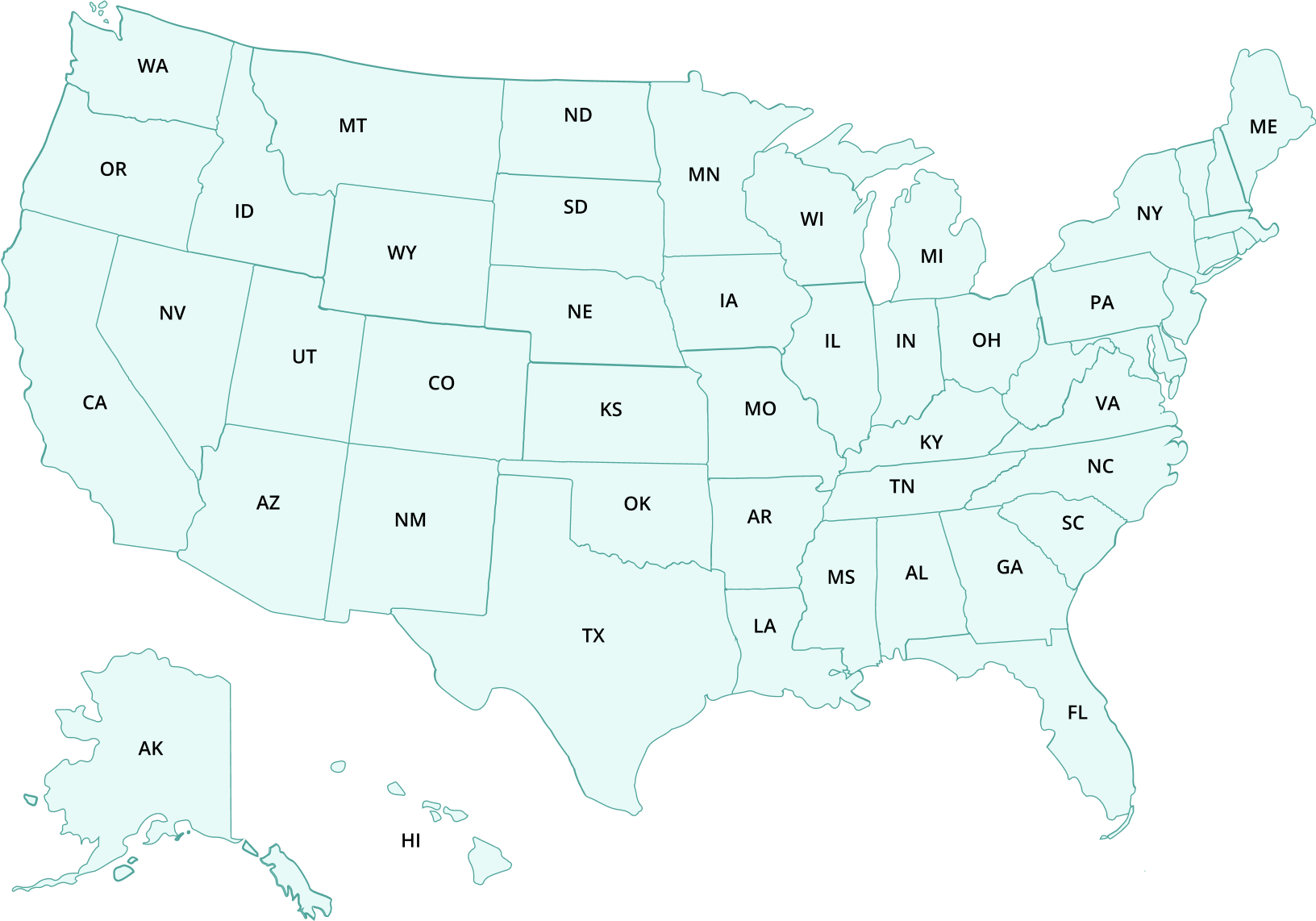
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- West Virginia
- Wisconsin
- Wyoming
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Page Sources
- Melemis, S. M. (2015). Focus: addiction: relapse prevention and the five rules of recovery. The Yale journal of biology and medicine, 88(3), 325. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553654/
- Substance Abuse: Clinical Issues in Intensive Outpatient Treatment. Treatment Improvement Protocol (TIP) Series, No. 47. Center for Substance Abuse Treatment.Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2006. Link: https://www.ncbi.nlm.nih.gov/books/NBK64094/
- Center for Substance Abuse Treatment. Substance Abuse: Clinical Issues in Intensive Outpatient Treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2006. (Treatment Improvement Protocol (TIP) Series, No. 47.) Chapter 4. Services in Intensive Outpatient Treatment Programs. https://www.ncbi.nlm.nih.gov/books/NBK64094/
- Larimer, M. E., Palmer, R. S., & Marlatt, G. A. (1999). Relapse prevention: An overview of Marlatt’s cognitive-behavioral model. Alcohol Research & Health, 23(2), 151. https://pubs.niaaa.nih.gov/publications/arh23-2/151-160.pdf
- Hendershot, C. S., Witkiewitz, K., George, W. H., & Marlatt, G. A. (2011). Relapse prevention for addictive behaviors. Substance abuse treatment, prevention, and policy, 6(1), 1-17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163190/
- Melemis S. M. (2015). Relapse Prevention and the Five Rules of Recovery. The Yale journal of biology and medicine, 88(3), 325–332. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4553654/
- Rampure, R., Inbaraj, L. R., Elizabeth, C. G., & Norman, G. (2019). Factors contributing to alcohol relapse in a rural population: Lessons from a camp-based de-addiction model from rural Karnataka. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine, 44(4), 307. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6881896/
- Schoenthaler, S. J., Blum, K., Braverman, E. R., Giordano, J., Thompson, B., Oscar-Berman, M., ... & Gold, M. S. (2015). NIDA-Drug Addiction Treatment Outcome Study (DATOS) relapse as a function of spirituality/religiosity. Journal of reward deficiency syndrome, 1(1), 36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455957/
- National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction Treatment and Recovery. July, 2020. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery

 Authored by
Authored by  Reviewed by
Reviewed by 
