Depression medication or antidepressant medications can help people live their best lives, but antidepressant side effects can sometimes make treatment unbearable. Out of 700 patients who took depression medicine, 38% of them reported experiencing side effects of antidepressants. Some of the common antidepressant side effects include lethargy, antidepressants weight gain, and digestive problems.
Table Of Contents:
However, a more serious side effect is sexual malfunction which could rob both couples and individuals of joy and fulfillment. Other depression medications can cause hair loss and health problems during pregnancy for both mother and baby. Fortunately, there are some medicines that are considered safe during pregnancy and this article will discuss them.
While some common side effects of antidepressants are mild and go away with time, others are long-lasting and even debilitating. Here is what people should know about the side effects of antidepressants.
More About Antidepressants:
What Are The Adverse Effects Of Depression Medications?
As common with most medicines, anti-depression medicines come with their own health risks which can be deadly if not managed properly. Side effects of antidepressants like nausea, insomnia, or headaches are common and could go away after a few weeks of taking the drugs. These are known as short-term after-effects and can last from a few days to weeks. On the contrary, long-term side effects of antidepressants can last for weeks and months (sometimes years). Examples of long-term side effects of antidepressants include weight gain, sexual problems, emotional numbness, suicidal thoughts, etc.
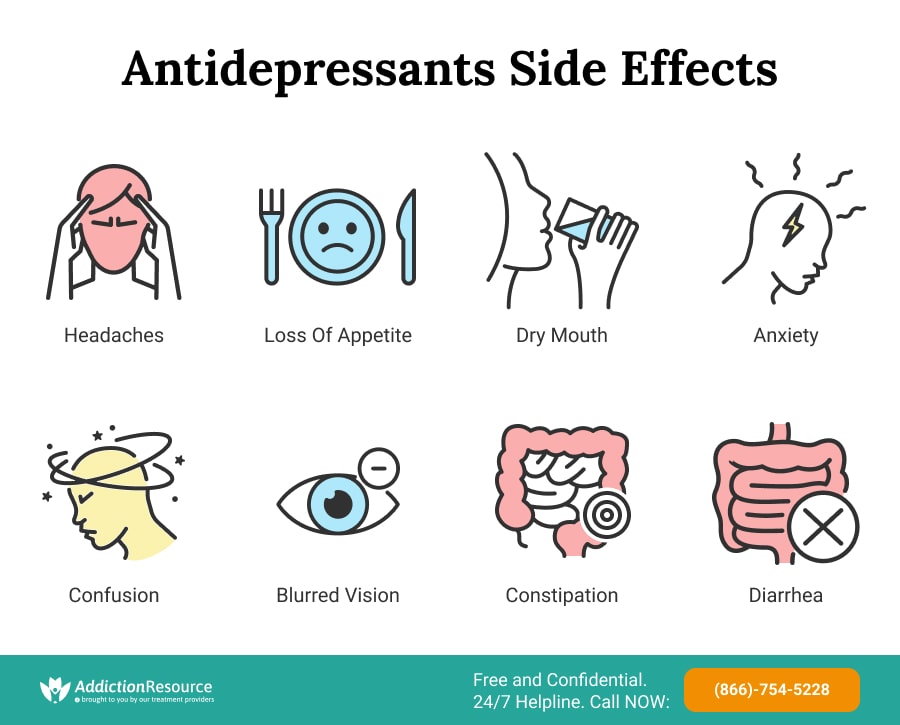
Short-Term Antidepressants Side Effects
As already mentioned, short-term antidepressant effects are adverse reactions that occur a few days to weeks after taking the drugs. Reports indicate that about 40% of patients suffer short-term effects. These adverse reactions, like dry mouth, disappear quickly after taking the medicines for a while. These adverse reactions can be categorized into physical and psychological side effects.
Physical Short-term Effects of Anti-depression Medicines:
- Weight fluctuations
- Headaches
- Nausea
- Loss of appetite
- Dry mouth
- Blurred vision
- Constipation
- Indigestion
Psychological Short-term Effects of Anti-depression Medication:
- Confusion
- Agitation
- Anxiety
- Irritability
These side effects are dependent on the particular class of anti-depression medication the patient is taking. Some may go away without additional treatment but others may require other drugs to help with the situation. It is best to consult a health professional once the symptoms begin for the best advice. This is to avoid complicating the already volatile health issues of the patient.

Long-Term Side Effects Of Antidepressants
As already stated, all antidepressant medications have both short-term and long-term effects. Many of these are mild, and most go away with time. However, some of these are so severe or long-lasting that patients end up needing to stop treatment due to side effects alone. TCA (antidepressants) tend to have the most effects. On the other end of the spectrum, medications on the SSRI antidepressants list have the least side effects. However, no depression medication is fully safe from causing negative symptoms of use. The long term effects of antidepressants can be classed into physical and psychological effects.
Physical Long-term Side Effects of Antidepressants:
- Hair loss
- Weight fluctuations
- Sexual problems
- Sleep disturbance
- Bleeding disorders
- Hyponatremia
- Diabetes mellitus
Psychological Long-term Side Effects of Antidepressants:
- Emotional numbness
- Inability to feel like themselves
- Caring less about other people
- Reduced positive feeling
- Feeling suicidal
- Reduced positive feeling
For those who are concerned about the aftereffects of depression medication in the long term, it is possible to be treated with options that are less likely to cause problems. Medications on an atypical antidepressants list and MAOI list tend to have relatively few side effects. There are also OTC antidepressants that can help people who prefer supplements to prescription drugs.
In any case, before using any drug or supplement, a doctor’s consultation is needed. Self-medication can lead to unpredictable health hazards, as well as an addiction that requires additional treatment.
Antidepressants and Sexual Problems
Depression medication’s sexual side effects can impact patients’ quality of life, decrease self-esteem, affect relationships, and even force patients to stop the medication. That’s why people need to know it is normal and expected that they discuss sexual issues with a doctor before and after starting an antidepressant. Studies show that men experience slightly more sexual side effects than women and that 40% of people who are under treatment with antidepressants will develop a form of sexual dysfunction at some point. Another study also revealed that 73% of people treated with SSRIs reported a significant decrease in libido. The study showed that the sexual problems were more common in men with 63% of the men reporting sexual dysfunction. Erectile dysfunction from depression medication is actually the most common reason for discontinuing antidepressants medicines. Other related symptoms are decreased interest in sex or the inability to reach an orgasm.
Other Adverse Effects Include:
- troubles with getting or maintaining an erection
- painful erection
- painful or delayed ejaculation
Reports indicate that women are twice as likely to take anti-depression medicine as men and these may have untold effects on their health. Antidepressant medication can affect women in many of the same ways, with decreased libido or the ability to achieve an orgasm. Though men are more affected, sexual problems in women caused by depression medicine are common. In a study of 107 people taking SSRIs, about 41% of women reported sexual dysfunction.
Other Common Sexual Side Effects in Women Include:
- lactation that is not caused by breastfeeding or pregnancy
- numbness in the nipples and vagina
- discomfort during sex
Women under serotonergic antidepressants treatment might experience blocked or delayed orgasm, delayed lubrication, or lack of interest in sex. Some medications for depression can also disrupt the menstrual cycle causing irregularities or changes in this process. Bupropion, Venlafaxine, and Fluoxetine can rarely cause menorrhagia (prolonged or heavy menstrual bleeding), while Bupropion might also cause menstrual spotting, shortened menstrual cycle, or the absence of menstruation.
The negative effects of antidepressants on the brain are a serious issue that must not be toyed with. Patients should stick to their treatment plan and report any issue to their health professionals for assistance.
Antidepressants Without Sexual Side Effects
Fortunately, there are antidepressants without sexual side effects that patients can utilize. These medications can help patients to enjoy their sex life while undergoing treatment. However, a doctor’s advice is required to choose the right medication for the patient.
Here is a list of antidepressants without sexual side effects:
- Bupropion
- Mirtazapine (Remeron)
- Amitriptyline
- Vortioxetine
- Vilazodone
- Nefazodone
These medicines are not selective serotonin reuptake inhibitors (SSRIs), thus they use other methods other than increasing serotonin in the brain. This helps to treat depression without affecting the sexual drives of patients. So, antidepressants and sex drive issues should not be the source of stress in relationships.
How to Increase Libido While on Antidepressants?
As already discovered antidepressants and sex drive have a strong connection with the medications severely affecting libido. This can be problematic and put unnecessary stress on any relationship. According to research on antidepressants and sex drive, 70% of people diagnosed with depression stand the risk of developing sexual problems. One way to avoid this problem is by switching to an antidepressant that has little to no effect on sexual drive. Another way is to add medicine that helps to improve libido. Patients can also lower the dose or engage in sexual activity when the effects of the antidepressants subside. Other means include taking a drug holiday or meeting a therapist to discuss ways by which one can overcome the psychological effects of sexual dysfunction.
Can Antidepressants Affect Your Period?
So, the million-dollar question is can antidepressants affect your period? It’s no news that some medications can affect women’s menstruation causing them to miss or have delayed periods. So are depression medicines part of medications that affect the period? Well, according to studies, some women have reported experiencing menstrual cramps, heavy bleeding, or totally missing their periods. Studies indicate that out of 793 women, 24.6% had menstrual disorders when they were on these medicines. So, anti-depression medication can affect a woman’s menstrual cycle.
Negative Effects of Antidepressants on the Brain
Medicines for depression can have negative effects on the brain if their usage is not properly checked. One of the negative effects of antidepressants on the brain is serotonin syndrome. This is due to the MOA of antidepressants when the serotonin levels in the brain rise to dangerous levels. This may lead to physical symptoms of serotonin syndrome such as diarrhea, sweating, and shivering. Also, one may experience psychological issues such as confusion, emotional instability and suicidal thoughts. The information available indicates that an increase in serotonin levels can cause mood swings and worsen anxiety which may lead to emotional instability and suicidal thoughts.
In a 2016 research on people taking drugs for depression, it was discovered that they endured the following psychological antidepressant side effects long term include:
- Feeling emotionally numb (72%)
- Inability to feel like themselves (54%)
- Reduced positive feelings (45%)
- Feelings of addiction (43%)
- Caring less about others (36%)
- Suicidal thoughts (36%)
The percentage sign next to the numbers indicates the percentage of people who complained of that particular after effect. Generally, the patients admitted to feeling less depressed, however, the antidepressant side effects long term kept rearing their heads. About 30% of the people surveyed also reported experiencing moderate to severe depression.

Antidepressants and Weight Gain or Loss
There is a direct link between antidepressants and weight gain with studies indicating that it normally occurs in the long term. According to a 2013 study in the Cleveland Clinic Journal of Medicine, the weight gain normally occurs after the patient had used the drugs for about 6 months. Research also showed that about 25% of people who took antidepressants reported weight gain. Thus, antidepressant side effects long term include weight gain. However, when it comes to weight loss, several studies show that bupropion was the only common antidepressant that caused weight loss.
Antidepressants and Hair Loss
One of the after-effects that is not often spoken about is antidepressant hair loss. Although not well-known, it is well-documented. Certain types of depression medication are more likely to lead to hair loss than others. For instance, a study revealed that out of a million taking ten different medicines for depression, it was discovered that those who took Wellbutrin run the risk of hair loss. So, those who are concerned about this negative effect of depression medicine could ask their doctor to prescribe one not associated with causing the hair to fall out.
However, the hair loss experienced from depression medication use is not permanent. It is called telogen effluvium, which is when the hair falls out due to stress on the body. Once the patient adjusts to the presence of the medication, hair loss side effects will stop, and the patches where the hair is missing will fill in again.
List of Antidepressants That Cause Hair Loss:
- Bupropion (Wellbutrin)
- Paxil (Paroxetine)
- Zoloft (Sertra hydrochloride)
- Prozac (Fluoxetine hydrochloride)
- Anafranil (Clomipramine)
- Janimine (Imipramine)
- Tofranil (Imipramine)
This may not be an exhaustive list of antidepressants that cause hair loss. There may be other medications that have a high risk of alopecia. Thus, patients should consult their medical doctors before taking any medicine to avoid future health issues. Hair loss is part of the rare long term effects of antidepressants and may strike a blow to a patient’s self-esteem but they should prioritize mental health. After all, it is just temporary and may go away as soon as the body adjusts to the medication.
Antidepressants and Pregnancy
Many women who deal with depression must take anti-depression medicines during pregnancy to keep the symptoms under control. There are pros and cons regarding the safety of taking these medications while pregnant, but research shows that most depression medications, especially SSRIs, are generally safe. However, studies also show that almost 30% of babies with mothers who took SSRIs during pregnancies will develop neonatal adaptation syndrome, which causes irritability, increased jitteriness, and difficulty breathing to name some of the side effects. Doctors are still not sure if the syndrome is caused by exposure to anti-depression medicines while pregnant or due to the baby’s withdrawal symptoms after birth.
There Are Some Other Risks Connected to Depression Medication and Pregnancy. Reported Risks for the Child Are:
- Miscarriage
- Birth defects (anencephaly, craniosynostosis, omphalocele, limb malformation)
- Heart defects
- Pulmonary hypertension
- Low Apgar scores
- Low birth weight
- Preterm birth
On the other hand, leaving the mother with untreated depression can be very dangerous to the mother, the unborn baby, and the mother’s family (other potential children). Women who suffer from depression are less willing to take care of themselves during pregnancy and are prone to risky behaviors, such as smoking, drinking alcohol, or taking drugs. Therefore, anti-depression medicines during pregnancy should be considered, among other options.
If the woman decides to change the treatment in the middle of pregnancy, due to concerns regarding the current medical treatment, this should be done only with the doctor’s advice. There are also some natural alternatives to antidepressants for mild forms of depression, which also need a doctor’s consultation before a pregnant woman starts taking them.
Safe Antidepressants While Pregnant
Studies indicate that about 2%-3% of pregnant women take antidepressant medicine while pregnant. The number increases to between 5%-7% after birth. Antidepressant medications can harm the fetus that is why it is necessary to know which ones are safer. Fortunately, there are several antidepressants that help with sleep and depression that pose a decreased risk in pregnancy and are considered safer. Studies indicate that SSRIs and SNRIs are considered to be safe antidepressants during pregnancy.
List of Safe Antidepressants During Pregnancy:
- Citalopram (Celexa)
- Bupropion (Wellbutrin)
- Fluoxetine (Sarafem, Prozac)
- Amitriptyline (Elavil)
- Nortriptyline (Pamelor)
- Sertraline (Zoloft)
- Desipramine (Norpramin)
It does not mean that the above-mentioned depression medications during pregnancy are 100% safe, they can pose health hazards as well. On the other side, different depression drugs can be safer. Everything depends on the case. That’s why it is critical to consult with a doctor and discuss possible options.
Can One Take Antidepressants While Breastfeeding?
Many women are reluctant when it comes to taking depression medicines while breastfeeding, but the treatment can be safely continued with careful monitoring of the baby and mother. Specialists do not encourage changing the effective medication for an untried one during the postnatal period, to avoid the risk of relapse. Women who are already taking antidepressants while pregnant are encouraged to continue it for at least six months after giving birth, to avoid a relapse of depression episodes. If the treatment is started during pregnancy, the mother should inform the doctor about her intention to breastfeed to develop the most appropriate treatment plan. A woman will be informed on how to get prescribed anti-depression drugs that will keep the baby safe.
Coping With Antidepressant Side Effects
If someone has severe depression, treating it may be more important than not experiencing adverse reactions, depending on what those reactions are. For individuals who wish to continue treatment despite the after-effects, learning how to cope with them is important. The first thing the patient should do is sit down with their doctor and determine if any of their other medications could be interacting in a way that produces adverse reactions of antidepressants. For example, antidepressants and birth control medications can interact to increase the likelihood of weight gain. The user could switch birth control drugs and eliminate this effect. From there, the user should look into strategies that can alleviate specific symptoms they are battling.
Here Are Other Ways a Patient Can Cope With the After-effects of Antidepressants:
- Engaging in less stressful physical exercises such as walking
- Taking short rests during the day
- Avoiding the operation of heavy machinery or driving until the fatigue is over
- Taking antidepressants at bedtime with the permission of your caregiver
- Consulting your medical doctor on reducing the dosage to help with the signs
It is up to the user to isolate the adverse reactions that are bothering them the most and then work with their doctor to figure out what strategies will bring them the most relief. However, all the steps should be taken under medical supervision only. Additionally, users should not attempt to self-medicate to address their symptoms as it can result in an overdose on antidepressants.
Always Seek A Doctor’s Advice
In a nutshell, antidepressants help treat depression but come with both short and long-term adverse reactions which include dry mouth, nausea, headaches, confusion etc. Long term effects of antidepressants are a result of using antidepressant medicine for a long time while short-term effects result from short use of antidepressant medicine. For example, one of the effects of long-term antidepressant effects is antidepressant addiction which can be linked to overdose on antidepressants. Hair loss can also be a result of long-term antidepressant use but it is temporary. Also, scientists have established a link between antidepressants and sex drive whereby the medications cause sexual problems.
However, there are several ways to improve libido including adding other medications or switching medicines. Though antidepressants are generally unsafe for pregnancy, SSRIs and SNRIs are considered safe to be used by pregnant women. Whether someone wishes to withdraw from antidepressants due to the negative effects of antidepressants, abuse of drugs, or just a desire to live pill-free, it is vital that the medicines are stops safely. Also, combining antidepressants and alcohol can be dangerous so patients must be wary. With a drug rehab center, withdrawal symptoms can be managed, and the medications tapered so that users feel little to no after-effects. It is possible to stop antidepressant use and still live a good life.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Page Sources
- Harvard Health Publishing. (n.d). Going Off Antidepressants. Harvard Health Publishing. https://www.health.harvard.edu/diseases-and-conditions/going-off-antidepressants
- C. Cartwright, K. Gibson, J. Read, O. Cowan, T. Dehar. (2016). Long-term Antidepressant Use: Patient Perspectives of Benefits and Adverse Effects. Patient Preference and Adherence.
- A. Higgins, M. Nash, A. Lynch. (2020). Antidepressant-associated Sexual Dysfunction: Impact, Effects, and Treatment. Drug Healthcare and Patient Safety.
- Am Fam Physician. (2004). Which Antidepressant Is Best to Avoid Sexual Dysfunction. Am Fam Physician. ://www.aafp.org/afp/2004/0515/p2419.html
- F. Uguz, M. Sahingoz, S. Kose, O. Ozbebit, C. Sengul, et al. (2012). Antidepressants and Menstruation Disorders in Women: A Cross-sectional Studies In Three Centers. Gen Hosp Psychiatry.
- M. Dubovicky, K. Belovicova, K. Csatlosova, E. Bogi. (2017). Risks of Using SSRI/SNRI Antidepressants During Pregnancy and Lactation. Interdisciplinary Toxicology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6096863/

 Authored by
Authored by  Reviewed by
Reviewed by 

