Antihistamines are some of the most popular drugs worldwide today. People are constantly getting allergic reactions to various things, and these medications are an easy way out. However, less common knowledge is that they can come with complications too – especially when taken long-term.
Table Of Contents:
- Why Do Antihistamines Cause Side Effects?
- What Are Antihistamine Side Effects?
- What Are First-Generation Antihistamine Side Effects?
- What Are Second-Generation Antihistamine Side Effects?
- What Antihistamine Precautions Are There?
- Can Antihistamines Be Taken During Pregnancy?
- Can Antihistamines Be Taken While Breastfeeding?
- What Are the Signs of Antihistamine Allergies and Intolerance?
- How Can Antihistamine Side Effects Be Reduced or Eliminated?

On that note, this text seeks to establish the connection between the mechanism of action of these drugs, and provide information about how side effects occur.
Why Do Antihistamines Cause Side Effects?
Allergic reactions occur when the body releases a substance called histamine. This substance binds to receptors on certain cells in the body, which in turn causes allergy symptoms. Antihistamines help to decrease these symptoms at the affected cell receptors.
Conversely, the actions of these medications in the body disrupt certain actions of the central nervous system, which can lead to complications too.
For instance, these antihistamine side effects are more likely to occur in older patients because they have lower numbers of cholinergic neurons in the brain, compromised renal and liver function, fewer cholinergic receptors, and a less stable blood-brain barrier. These are all body functions that antihistamines disrupt while in action.
What Are Antihistamine Side Effects?
Certain types are more likely to cause complications than others. For instance, the first generation is more likely to cause complications such as drowsiness than the second generation. Also, the long-term effects of antihistamines tend to cause more problems such as overdose and addiction.
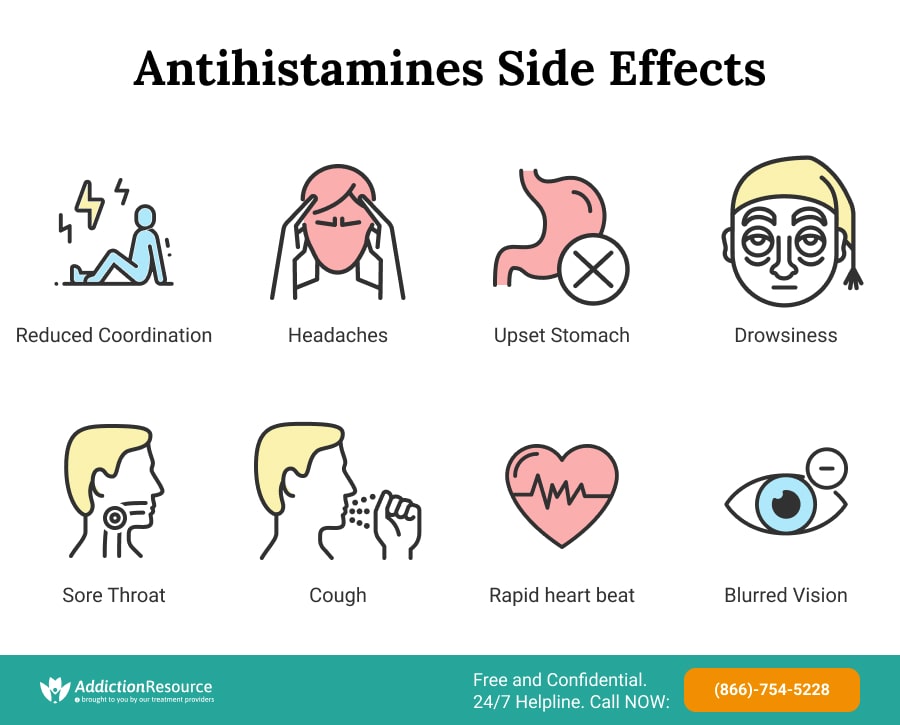
Some Known Antihistamines Side Effects Include:
- Reduced coordination
- Blurred vision
- Difficulty peeing
- Dry mouth, nose, or throat
- Headache
- Drowsiness
- Dizziness
- Increased appetite and weight gain
- Thickening of mucus
- Upset stomach
- Low blood pressure
- Rapid heart rate
- Cough
- Tiredness
- Sore throat
- Abdominal/muscular/joint pain or discomfort
First-Generation Antihistamine Side Effects
When comparing first-generation and second-generation options, older medications tend to come with significantly more complications. Not only that, but they tend to have more severe expressions and occur more often in users than their newer counterparts.
Common Side Effects of Antihistamines of the First Generation Include:
- Sedation
- Dizziness
- Blurred vision
- Headache
- Poor coordination
- Blood pressure fluctuations
- Dry Mouth or nose
- Dry Eyes
- Mucus thickening in the airways
- Difficulty with urination
- Rapid heart rate
From all the possible complications, the most common is sedation and other central nervous system-related symptoms. This category of effects affects at least 20% of patients. including dry mouth or nose and difficulty with urination.
In general, whenever possible, first-generation medications should be avoided due to these potentially severe complications.
Second-Generation Antihistamine Side Effects
Second-generation versions (non-drowsy antihistamines) adverse reactions are not as numerous as those of their first-generation counterparts. When they are expressed, they tend not to be as severe.
However, there is still a possibility that complications will manifest, and if this happens, it is important to check with a healthcare professional to know what the right steps to take are. These professionals will help to determine if the reactions can be managed, or if one must stop taking the drug.
For the second generation, do antihistamines make you sleepy? While this category is marketed as non-drowsy antihistamines, sleepiness is still a side effect they can cause. Antihistamines and blood pressure changes are also a possibility.
Other Complications Common to These Medications Include:
- Fatigue
- Headache
- Nausea
- Dry mouth or nose
- Cough
- Tiredness
- Vomiting
- Sore Throat
- Abdominal pain/discomfort
Most users find that the side effects of antihistamines are easy to deal with, but some patients may find them intolerable. Despite being over the counter, users should discuss the medications with their doctor to determine which ones are best for them.
Summarily, this information shows that there are significant differences between the first-generation and second-generation, even though they are both technically taken for similar purposes. The differences are important enough that one needs to be well-informed before taking any type of drug. It is important to avoid self-medication.
It is also crucial to point out that the lists mentioned here are inexhaustive, and it is possible to experience symptoms that have not been listed. If this occurs, contact a doctor or pharmacist for professional medical advice as soon as possible.
What Are the Precautions?
They might be made for medical treatments, but these drugs are not to be taken without precautions. These precautions typically center around people living with specific conditions, as these conditions may affect the mechanism of action in the body, or cause harm through drug interactions.
On that note, individuals should discuss usage with their doctor before taking allergy medication.
These Precautions Are:
- Patients with QTc prolongation (increased risk of potentially fatal cardiac arrhythmias)
- Women who are lactating
- People with impaired renal or hepatic function
- Hypertension
- Urinary retention
- Cardiovascular disease
- Increased ocular pressure

It should also be noted that studies are showing that dementia could be one of the long-term effects of antihistamines on health. As such, older adults may need to avoid these allergy medications.
Antihistamines and Pregnancy
Studies show that during pregnancy, 10% to 30% of women with pre-existing allergic rhinitis noticed an increase in symptoms. The same studies also showed that the increased symptoms can be well-managed with the right options.
What then is the relationship between antihistamine and pregnancy? What is the right type to use during pregnancy? Read further to know.
Antihistamines That Are Safe During Pregnancy
Antihistamine and pregnancy are particularly safe when some of the oral variants are taken, along with some nasal sprays and steroid nasal sprays.
Nasal sprays are deemed safe because their mechanism of action does not require traveling through the entire body where other organs or body functions could be impacted.
Here Is a List of Options That Are Considered Safe During Pregnancy:
- Chlorpheniramine
- Dexchlorpheniramine
- Levocabastine eye drops (Livostin)
- Azelastine nasal sprays (Astelin, Astepro)
- Hydroxyzine (Atarax, Vistaril)
- Desloratadine (Clarinex)
- Emedastine eye drops (Emadine)
- Levocabastine oral (Xyzal)
Antihistamines That Are Dangerous During Pregnancy
There is not enough research to back up the possibility of increased risk involving antihistamine and pregnancy. The report from the Center for Disease Control and Prevention is the closest bit of information to answer the question, and it showed that only 9 out of 54 studies suggested possible risks which still require further investigation.
The lack of strong research on the matter means that these situations should be treated on a case-by-case basis, as a personal consultation with a doctor will provide a more definitive answer about what to avoid.
Skipping Antihistamines During Pregnancy
If a patient’s allergy symptoms are bad enough that they are causing problems (such as finding it hard to sleep), then taking these drugs while nursing will benefit both the user and the baby’s health.
For instance, proper medication should be taken as prescribed if there are symptoms of allergic asthma. During pregnancy, uncontrolled asthma can cause serious complications. Considering the fact that existing asthma symptoms flare by up to 45% in pregnant women, it is important to have knowledge of how to control the situation ahead of time.
Complications that may occur as a result of uncontrolled asthma during pregnancy include:
- Increased risk of cesarean section
- Gestational diabetes
- Hemorrhage
- Placenta abruption
- Placenta previa
- Premature rupture of membranes

Thus, asthma is one of the conditions that almost certainly require allergy medications. However, the onus lies on the doctor to decide if alternatives can be taken for cases where the allergy can be managed through other means.
Possible Congenital Disabilities Associated With Antihistamine Use
In a CDC study, researchers gathered information from over 50 scientific submissions to see if usage of these drugs during pregnancy showed any risk of possible congenital disabilities or disease.
The Evidence Found Showed These Facts:
- Scientific research deems most of them are safe during pregnancy since they are not related to any congenital disabilities or disease.
- There were 9 out of 54 potential links between these medications and congenital disabilities/disease, which need to be studied further.
- More studies were found on anti-allergens that were commonly used to treat nausea, allergies, asthma, or vomiting with drugs like loratadine, dimenhydrinate, cetirizine, and diphenhydramine.
- On the other hand, there were relatively lesser studies on the drugs that were taken to treat indigestion, such as ranitidine, cimetidine, or famotidine.
Antihistamine and Breastfeeding
Allergies are already difficult enough for regular people to cope with, and the discomfort that comes with having them is even greater with pregnant and breastfeeding mothers. When a breastfeeding mother is showing allergic symptoms, it can call for an antihistamine to manage and control the symptoms.
This leads to the question – is the interaction of antihistamine and breastfeeding safe? Evidence suggests that there is not much to worry about in this regard, but some care must be taken. Information about how the different types (sedating and non-sedating) can be used safely while breastfeeding is discussed below.
Non-sedating
Any non-sedating anti-allergen, such as cetirizine or loratadine, shows shallow levels of transfer to the breast milk and hence should be considered the best option while breastfeeding.
There is not enough evidence to present other non-sedating options as safe while breastfeeding, but based on the evidence on hand for pharmacology, there shouldn’t be any problem. Therefore, it would be safe to use them during breastfeeding, but with caution and always approval from the doctor.
Sedating
Adverse reactions can be seen in a breastfeeding infant, like irritability and drowsiness caused by the use of sedating anti-allergens. Cyproheptadine has potential effects on lactation, which is why it is contraindicated in breastfeeding.
There is evidence to back this up in a study conducted in 2010, but the study also showed that the instances where these drugs had a health effect on the infant did not require medical attention. Therefore, the possibility of sedation that comes with using this category is not a cause for worry in the short-term interaction of antihistamine and breastfeeding.
If the prescription required is a long-term one, the drug may still be administered but it must be used with close monitoring of the situation of the mother and child.
Signs of Antihistamine Allergies and Intolerance
These medications treat allergies, so it may seem strange that people can be allergic to, intolerant of, or hypersensitive to them. However, this does occur. People who are allergic to antihistamine drugs may be unable to take any drug in the class, or they may only have problems with a specific type.
Allergies to these medications can be hard to diagnose since the symptoms can mimic the condition they are meant to treat.
Signs of Allergies and Intolerance to These Medications Include:
- Skin rash
- Hives
- Itching
- Fever
- Swelling
- Shortness of breath
- Wheezing
- Runny nose
- Itchy, watery eyes
- Itchy ears
- Tightening of the throat and chest
- Trouble breathing
- Nausea
- Abdominal cramps
- Vomiting or diarrhea
- Dizziness or lightheadedness
- Changes in pulse
- Drop-in blood pressure
- Seizure
- Loss of consciousness
Instances of these allergic reactions are not rampant, especially considering that one of the key functions of the medication is to manage allergies. This means that the symptoms listed above are not common, and only surface in a few cases.
However, any allergic reaction must be addressed by immediately stopping usage of the medication, followed by consultation with a doctor. Even though they are rare, the instances where they do occur can be severe.
How to Reduce or Eliminate Antihistamine Side Effects
The best way to reduce or eliminate side effects is to take the drug as recommended and not to take it long-term unless necessary. Whenever possible, users should take non-sedating options over first-generation options. However, it is not always possible to reduce or eliminate antihistamine side effects.
For those who take their medications as directed and still have uncomfortable complications, a natural alternative might be best. Another option would be non-antihistamine allergy medicines. Users can weigh the difference between these and decongestant medications to determine if one might better suit them than the other. However, as always, they should discuss all medications with their doctor first.
General side effects on health are not the only risk that comes with taking these medications; abuse and addiction can also occur. Anyone who is misusing allergy medications should seek medical help and treatment. Addiction rehab centers offer the right solutions to stop use and live a better life.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Page Sources
- Shakouri AA, Bahna SL. Hypersensitivity to antihistamines. Allergy Asthma Proc. 2013 Nov-Dec;34(6):488-96. https://www.ncbi.nlm.nih.gov/pubmed/24169055
- Ozdemir PG, Karadag AS, Selvi Y, Boysan M, Bilgili SG, Aydin A, Onder S. Assessment of the effects of antihistamine drugs on mood, sleep quality, sleepiness, and dream anxiety. Int J Psychiatry Clin Pract. 2014 Aug;18(3):161-8. https://www.ncbi.nlm.nih.gov/pubmed/24673474
- So, M., Bozzo, P., Inoue, M., & Einarson, A. (2010). Safety of antihistamines during pregnancy and lactation. Canadian family physician Medecin de famille canadien, 56(5), 427–429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2868610/
- Simons, F. E., & Simons, K. J. (2008). H1 antihistamines: current status and future directions. The World Allergy Organization Journal, 1(9), 145–155. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3650962/
- Church, M. K., & Church, D. S. (2013). Pharmacology of antihistamines. Indian journal of dermatology, 58(3), 219–224. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3667286/
- Wong H. (2015). Long-term use of diphenhydramine. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 187(14), 1078. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4592307/
- Farzam K, Sabir S, O'Rourke MC. Antihistamines. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. https://www.ncbi.nlm.nih.gov/books/NBK538188/
- Murphy V. E. (2015). Managing asthma in pregnancy. Breathe (Sheffield, England), 11(4), 258–267. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4818212/
- Gilboa SM, Ailes EC, Rai R, Anderson J, Honein MA. Antihistamines and Birth Defects: A Systematic Review of the Literature. Expert Opinion on Drug Safety. 2014. https://www.cdc.gov/pregnancy/meds/treatingfortwo/features/antihistamines-and-bd.html
- Hindmarch, I., & Shamsi, Z. (1999). Antihistamines: models to assess sedative properties, assessment of sedation, safety, and other side‐effects. Clinical & Experimental Allergy, 29, 133-142. https://onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2222.1999.0290s3133.x

 Authored by
Authored by  Reviewed by
Reviewed by 









