Deaths caused by excessive alcohol use increased an alarming 29% in the U.S. over the past five years, placing alcohol as a silent killer.
As the liver is the primary site of ethanol metabolism, it’s the organ that usually sustains the most significant degree of tissue injury by heavy drinking. Hepatic lesions can take up to a decade to progress, often without presenting symptoms, making them easy to overlook in primary care settings.
Keep reading to learn about alcoholic liver disease, its symptoms and stages, and how to get help before it becomes too late.
Table Of Contents:
What is Alcohol-Related Liver Disease (ALD)?
Alcohol-induced liver diseases include a range of hepatic conditions, starting with fatty liver, progressing to alcoholic hepatitis, and ending in alcoholic cirrhosis —the most advanced and irreversible form of liver damage due to heavy alcohol consumption.
Alcohol is the primary cause of liver disease worldwide, and evidence suggests that the type of alcohol consumed may influence the risk of developing liver disease.
Alcoholic Liver Disease Stages
The spectrum of alcohol-related liver injury varies from simple steatosis to cirrhosis. These stages are not necessarily distinct phases of the liver disease evolution but rather represent multiple concurrent stages in an individual.
They are commonly grouped into three stages of ALD: 1) fatty liver or simple steatosis, 2) alcoholic hepatitis, and 3) chronic hepatitis with hepatic fibrosis or cirrhosis. Understanding these stages is crucial for the diagnosis, treatment, and management of alcohol-induced liver disease.
| Stage | Description | Symptoms | Causes |
|---|---|---|---|
| Fatty Liver (Steatosis) | Accumulation of fat in the liver cells due to alcohol consumption | Often asymptomatic; fatigue, abdominal discomfort. 100% potentially reversible with 4-6 weeks abstinence. | Present in 90% of individuals who drink more than 60 g/day of alcohol |
| Alcoholic Hepatitis | Inflammation and liver cell damage caused by alcohol abuse | Jaundice, abdominal pain, fever, nausea, vomiting fever, increased thirst | Prolonged and excessive alcohol intake; binge drinking |
| Hepatic Fibrosis (Cirrhosis) | Severe scarring of liver tissue, irreversible damage | Ascites (abdominal swelling), jaundice, severe fatigue, appetite loss, spider angiomas | Long-term chronic and severe alcohol abuse; typically, 10-20 years of heavy drinking |
Causes of Alcoholic Liver Disease
Alcohol-induced liver disease is primarily caused by excessive and prolonged alcohol consumption. The liver metabolizes alcohol, and chronic heavy drinking can overpower its capacity, leading to various forms of liver damage.
Besides heavy alcohol consumption, other main factors influencing the disease may be:
Genetic Factors
Studies have already identified gene variations associated with higher susceptibility to ALD, including genes that control inflammation and alcohol metabolism.
People with these genetic variations are more vulnerable to liver damage from alcohol.
Pattern of Drinking and Duration of Alcohol Use
Binge drinking or consuming large amounts of alcohol in a short time can significantly increase the risk of developing ALD, as it puts stress on the liver and increases the likelihood of liver inflammation and injury.
Gender
Due to differences in body composition, metabolism, and liver enzyme activity, a woman’s body is more susceptible to alcohol-related liver damage, even with lesser alcohol exposure. For example, the risk of developing cirrhosis is higher in men taking 60-80 g/day of alcohol for ten years or longer in men, but it takes 20g/day in women.
Nutritional and Lifestyle Factors
Chronic alcohol intake is associated with deficiencies of many micronutrients, such as thiamine, folate, pyridoxine, vitamin A, vitamin D, zinc and iron.
Most of the medical manifestations of alcoholic liver disease are related to vitamin deficiencies. A high-calorie diet causing obesity, as well as smoking, can also aggravate the effects of alcohol on the liver.
Other Health Conditions
Viral infections, which are concurrent liver diseases, such as hepatitis C and hepatitis B, as well as fatty liver disease, can cause rapid progression to fibrosis, cirrhosis, and even hepatocellular carcinoma.
Alcoholic Liver Disease Treatment
The primary focus to treat alcohol-related liver disease is 100% alcohol cessation and supportive care, although advanced stages may require additional interventions.
After medical screenings such as liver function tests (LFTs), complete blood count (CBC), FibroScan, or even a liver biopsy, a multidisciplinary team may follow the next series of treatments:
Nutritional Support and Lifestyle Changes
After patients have undergone alcohol detox, they receive medical and psychological support to help them overcome alcohol dependence; nutritional support and lifestyle change guidance may be included along with supplementation to improve liver function.
Medications
- Corticosteroids to reduce liver inflammation and improve survival rates in severe cases of alcoholic hepatitis
- Pentoxifylline to reduce inflammation and improve liver function
- Ursodeoxycholic Acid (UDCA) enhances bile flow and protects liver cells in some instances of ALD
Management of Complications
A couple of health complications can be caused by alcoholic liver disease. In severe cases, ascites are managed with diuretics, dietary sodium limits, fluid removal, or shunt placement.
Hepatic encephalopathy is treated with ammonia-reducing medications like lactulose or rifaximin. Variceal bleeding is treated with medications and procedures like banding or sclerotherapy.
Liver Transplantation
In advanced cases of ALD with irreversible liver damage (cirrhosis), liver transplantation may be considered. This involves replacing the diseased liver with a healthy liver from a deceased or living donor.
Alcohol-Related Liver Disease – Prognosis and Final Considerations
As ALD is a complex diagnosis, identifying underlying factors such as depression or post-traumatic trauma contributing to alcohol use disorder is a crucial action.
While early-stage liver disease prognosis is favorable with alcohol abstinence, up to 20% of patients may progress to irreversible cirrhosis. At this stage, a multidisciplinary team is crucial for optimal treatment or supportive care. Screening for hepatocellular carcinoma is essential.
Preventing serious diseases like ALD requires awareness of one’s habits and lifestyle. If you or someone you know is concerned about potential alcohol dependence, promptly seek help from addiction specialists.
People Also Ask
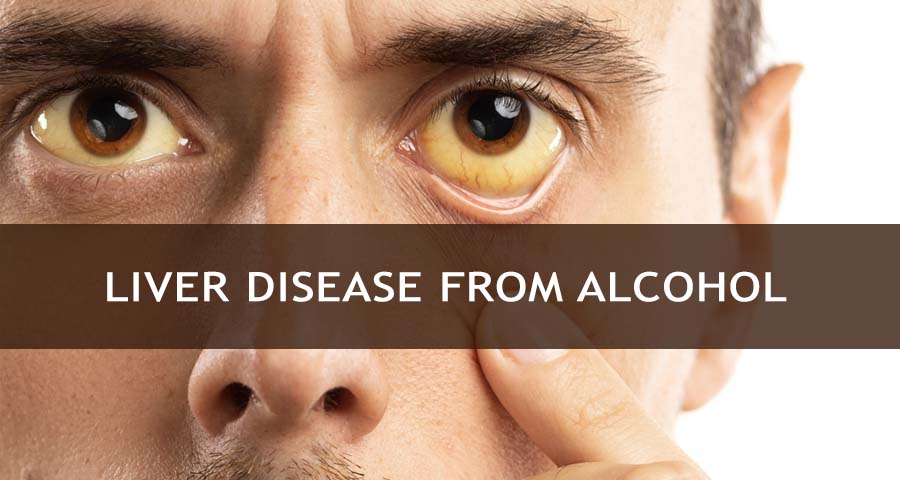
What are the first signs of alcoholic liver disease?
Early signs of alcohol-induced liver disease include fatigue, jaundice (yellowing of the skin and eyes), abdominal pain, swelling in the abdomen, nausea, and loss of appetite. Early detection and intervention are crucial for managing the condition.
How does alcohol affect the liver?
Alcohol affects the liver by causing damage and impairing its functions. Excessive or chronic alcohol consumption can lead to conditions such as fatty liver disease, alcoholic hepatitis, fibrosis, and cirrhosis. Additionally, alcohol impairs the liver’s ability to regulate blood sugar levels and produce essential proteins. Moderating alcohol intake is crucial for maintaining liver health and preventing alcohol-related liver diseases.
Can alcoholic liver disease be cured?
Alcohol-related liver disease can be managed and potentially reversed through abstaining from alcohol, adopting a healthy lifestyle, and receiving medical treatment. However, severe damage may be irreversible, requiring ongoing management to prevent further deterioration.
What are the three stages of alcoholic liver disease?
The three stages of alcohol-induced liver disease are fatty liver (steatosis), alcoholic hepatitis, and cirrhosis. These stages represent a progression of liver damage, with cirrhosis being the most severe and potentially life-threatening stage.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Find Drug Rehabilitation Centers Near You Anywhere In the US
Addiction Resource team has compiled an extensive list of the top drug rehabilitation facilities around the country. Use our locator tool to find the best centers near you.
Page Sources
- Esser, M. B., Sherk, A., Liu, Y., & Naimi, T. S. (2024). Deaths from Excessive Alcohol Use — United States, 2016–2021. Morbidity and Mortality Weekly Report, 73(8), 154–161. https://doi.org/10.15585/mmwr.mm7308a1
- Hazeldine, S., Hydes, T., & Sheron, N. (2015). Alcoholic liver disease – the extent of the problem and what you can do about it. Clinical Medicine, 15(2), 179-185. https://doi.org/10.7861/clinmedicine.15-2-179
- Patel, R., & Mueller, M. (2023, July 13). Alcoholic liver disease. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546632/
- Maher, J. J. (1997). Exploring Alcohol’s Effects on Liver Function. Alcohol Health and Research World, 21(1), 5-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6826796/
- Dasarathy, S., & McCullough, A. J. (2010). Alcoholic liver disease. Hepatology, 51(1), 307-328. https://doi.org/10.1002/hep.23258
- Meroni, M., Longo, M., Rametta, R., & Dongiovanni, P. (2018). Genetic and Epigenetic Modifiers of Alcoholic Liver Disease. International Journal of Molecular Sciences, 19(12). https://doi.org/10.3390/ijms19123857
- Kezer, C. A., Simonetto, D. A., & Shah, V. H. (2021). Sex differences in alcohol consumption and Alcohol-Associated liver disease. Mayo Clinic Proceedings, 96(4), 1006–1016. https://doi.org/10.1016/j.mayocp.2020.08.020
- Halsted, C., & Medici, V. (2016). Alcohol: Metabolism and Health Effects. Encyclopedia of Food and Health, 82-87. https://doi.org/10.1016/B978-0-12-384947-2.00018-0
- Singal, A. K., Walia, I., Singal, A., & Soloway, R. D. (2011). Corticosteroids and pentoxifylline for the treatment of alcoholic hepatitis: Current status. World Journal of Hepatology, 3(8), 205-210. https://doi.org/10.4254/wjh.v3.i8.205
- Achufusi, T. G. O., Safadi, A. O., & Mahabadi, N. (2023, February 12). Ursodeoxycholic acid. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK545303/
- Paik, H., Lee, K. S., Han, H., Song, K. H., Kim, M. H., Moon, B. S., Ahn, S. H., Lee, S. J., Park, H. J., Lee, D. K., Chon, C. Y., Lee, S. I., & Moon, Y. M. (2005). Comparison of Rifaximin and Lactulose for the Treatment of Hepatic Encephalopathy: A Prospective Randomized Study. Yonsei Medical Journal, 46(3), 399-407. https://doi.org/10.3349/ymj.2005.46.3.399
- Osna, N. A., & Kharbanda, K. K. (2017). Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol Research : Current Reviews, 38(2), 147-161. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513682/


 Reviewed by:
Reviewed by:  Written by:
Written by: 
 FindTreatment.gov
FindTreatment.gov