Opioids are prescription substances that help with pain management by producing pain-relieving and euphoric effects. Although opioids drugs provide temporary relief to the user, opioid side effects can affect a patient’s well-being. According to a study published in The American Journal of Emergency Medicine, 95% of opioid users experience opioid induced constipation. Aside from this, there are other side effects of opioids that can be risky in both short-term and long-term use. Thus, proper management of these adverse opioid effects through some professional resources is necessary.
Table Of Contents:
In this article, information about the common and long-term opioid side effects, the dangers of taking opioid medications during pregnancy, substances that interact with opioids, and how to manage opioid effects such as opioid induced constipation treatment will be provided.
More About Opioids:
What Are The Common Side Effects Of Opioids?
According to a clinical review of medical doctors from the United States, all patients using opioids, either prescription or illicit ones, are expected to experience common opioids side effects. In the same study, it was also reported that the severity of these opioids side effects is dose-dependent.
Opioid Induced Constipation
According to a clinical review published in the American Family Physician, opioid induced constipation is the most common side effect of opioids, with a prevalence rate of 40-95%. Taking them regularly can lead to a change in bowel movements, and thus the user may suffer from stomach issues, such as opioid constipation, for the period in which they were used. In the same study, it was reported that even a single opioid dose can already cause this reaction. Additionally, when opioid induced constipation occurs, a person may experience additional symptoms after they use the drug. Thus, individuals should also look out for the accompanying symptoms to understand whether the opioid drugs that they have taken caused them to experience these side effects.
Specific Symptoms That a Person Should Look Out for Include:
- The stool may be dry and hard
- Some people may experience nausea
- In more serious cases of opioid constipation, vomiting may also occur
- Abdominal tenderness
- Defecating may cause pain and strain
- Bloating
- The abdomen may bulge
- Distension
- Tiredness may develop in some people, along with lethargy
- Appetite loss
The scientific research on opioid induced constipation explains that opioid constipation is diagnosed when a person passes less than three stools for one week, which may be a sign that a person has developed this side effect as a result of opioid usage. The period during which opioid induced constipation will last depends from one person to another. Several factors should be taken into account in the particular scenario, which will have a potential impact on whether or not a person will become constipated, and for how long. OIC is more likely to occur in patients who use pain-relieving medicine for prolonged durations.
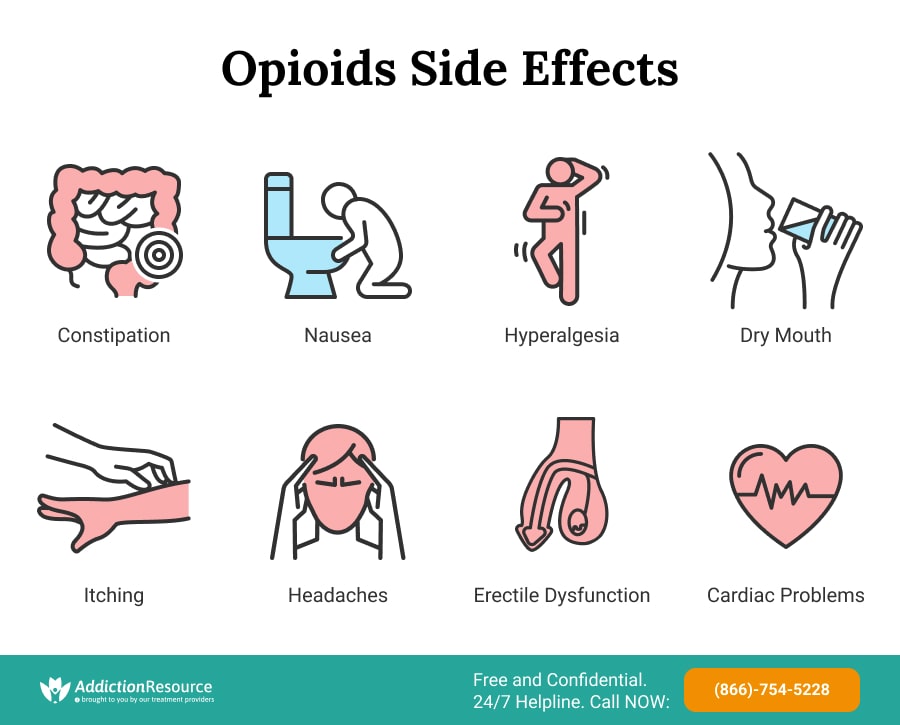
Drug Induced Nausea
Followed by opioid constipation, one side effect of opioid medications that often appears as stomach discomfort and the sensation of vomiting is called nausea. According to a study of doctors from New York, this side effect is also dose-dependent and it can lead to a lack of appetite and deteriorating health, consequently. In another study published in the Journal of Pain and Symptom Management, this nausea is a short-term effect and can subside within 2-3 days.
Drug Related Dizziness
According to a study of physicians from Japan, another common side effect of opioid drugs is dizziness. The euphoric effect of the substance is likely to make the user feel tired and sleepy. In the same study, it was also reported that the elderly are most at risk of experiencing this side effect. As a result, the user may sleep for long periods (until the effect of the pill wears off). Extreme dizziness is known among the signs of opioid overdose. This condition can be deadly and requires immediate professional care.
Opioid Induced Hyperalgesia
According to a study of scientists from Italy, opioid induced hyperalgesia is perhaps the riskiest side effect of opioids. Opioid induced hyperalgesia refers to a condition where taking a high dose results in a lowering of pain threshold. As a result, the pain worsens and becomes unmanageable even with accelerating the doses. Additionally, although opioid induced hyperalgesia is considered common, if there is no proper management, opioid induced hyperalgesia could lead to cell death. The user may also experience unusual pain symptoms such as allodynia. If the current medication isn’t working anymore, a patient should ask a doctor to use opioid conversion for switching the medicine.
Drug Related Dry Mouth
Frequent use may also lead to less production of saliva in salivary glands. According to a study of a doctor from Chicago, opioids could cause xerostomia or hyposalivation which can be experienced by almost all opioid users, especially females. As a result, the user may have a parched sensation in the mouth. In another study by physicians from Germany, the drug dihydrocodeine is reported to cause xerostomia in 80% of its users. Lastly, according to a clinical review of scientists from New Zealand, the opioid analgesic Tramadol may also cause dry mouth in 6.1% of patients using it.
Itching and Other Allergies
According to a study of doctors from the USA, another common opioid side effect is allergic reactions with a prevalence rate of 8.9%. In some cases, this results in opioid itching, which can cause discomfort. Although this is not a life-threatening effect, the user must consult the doctor and seek care about this side effect, even if a mild symptom is observed to avoid other complications.
Opioid Induced Headaches
This is one of the other most common opioid side effects. It might sound ironic that a substance used to relieve pain causes a headache – but it’s true. According to a study of physicians from Pennsylvania, headaches caused by this medication are known as rebound headaches. These are some common side effects of opioids experienced in the short term as they may only last for less than 10 days. However, chronic consumption can pose a severe threat to the health of the user.
To avoid the harmful opioid side effects, one may look for over-the-counter opioids and remember that the dosage must be administered very carefully.
Long-Term Side Effects Of Opioids
Long-term use of opioid medications causes complications. According to a study of medical doctors from Philadelphia, aside from dependence and tolerance, those who abuse and misuse opioids are at risk of developing an addiction. Other opioid or opiate serious side effects on the user’s health are listed in the information below.
Opioid Erectile Dysfunction
One of the opioid side effects on prolonged use is erectile dysfunction. The research found out that men who were using them were about 50% more likely to experience sexual dysfunction as a side effect as compared to those who do not use this medication. Opioid substances do not only interfere with the production of testosterone but also lessen interest, excitement, and sensation – resulting in erectile dysfunction in men.
Medication Related Cardiac Problems
Cardiac problems associated with opioid use are rare. Although no direct link between opioid usage and chronic heart failure has been established, there are many severe cardiac problems linked to the long-term side effects of opioids, including impaired functioning of the heart muscle, slower heart rate, and dilation of blood vessels. Apart from these, ventricular tachycardia, a type of cardiac arrhythmia, atrial fibrillation, and infectious endocarditis are also fairly common heart side effects associated with prolonged use.
Drug Induced Kidney Damage
Long-term side effects of opioids can result in chronic kidney damage. This is because it leads to a decrease in fluid intake, which can result in severe dehydration (if not noticed early). Furthermore, by causing multiple interruptions in the micturition reflex, opioid side effects can result in urinary retention, where a significant amount of residual urine is left behind due to impaired emptying of the bladder. Both of these factors lead to kidney damage.
Opioid Respiratory Depression
How do opioids cause respiratory depression? According to a clinical research of physicians from the Netherlands, prolonged use of these medications can alter the functioning of specific components of the user’s central nervous system, including the pre-Bötzinger complex, a respiratory rhythm generating area in the pons. This is called opioid respiratory depression. Use of drugs that activate the mu-opioid receptor cause analgesia linked to respiratory depression. Different medicine contains different amounts of opioids. Thus, their effect on the respiratory system varies.
Opioid Addiction And Abuse
Perhaps the most dangerous side effect of opioids linked to prolonged use is addiction. Since they produce pleasurable and euphoric effects, they are highly addictive and thus, chronic consumption of this substance – especially in the form of drugs – can lead to abuse and addiction. This is a grave issue, which can cause severe physical and mental problems.
If some signs of abuse are noticed in a patient, they should immediately seek resources such as addiction treatment for opioids. This condition brings severe risks because the user becomes highly dependent on the drug and loses control of the senses and body when opioid tolerance and withdrawal occurs. Addiction can end up lethal. According to opioid crisis statistics, around 72000 people died in the US in 2017 due to opioid addiction.

Opioids And Pregnancy: Taking Opioids While Pregnant
According to the Centers for Disease and Control Prevention, seeing the harmful side effects of painkillers, pregnant, and breastfeeding women are advised not to take any medicines without consulting a doctor. During pregnancy, a woman’s body undergoes massive hormonal changes, and it is likely to react to medication differently than under normal circumstances. Thus, it can be said that pregnant and breastfeeding women are at a higher risk of suffering from the dangerous adverse effects of opioids.
The use of painkillers, such as Oxycodone, Hydrocodone, Codeine, Hydromorphone, and Fentanyl, must be strictly avoided during pregnancy. These drugs are categorized as Pregnancy Category C where studies have found significant adverse effects on the fetus. Furthermore, these pills are also highly addictive and prolonged use of opioids in pregnancy can lead to addiction. Pregnant women with this disorder are most at increased risk of serious complications, including placental abruption, abnormal fetal growth, premature birth, and stillbirth in extreme cases.
Regular usage of these meds is not safe for infants on breastfeeding as well. Generally, if the amount of a sedative drug excreted in breast milk is less than 10%, it is considered safe for the infant. It depends on opioids half life and patients’ features. However, in the case of codeine and oxycodone, the infant is at risk of sedation even if the amount is less than 10%. As a result, prolonged use of opiates can adversely affect the infant’s central nervous system (CNS). Mothers who use these drugs must keep an eye on their breastfed infants for signs of CNS depression. For pregnant women who wish to wean off opioids, considering resources such as drug or medical intervention would be a great option.
Opioids Interactions: What Are The Dangers And Adverse Reactions?
Opioids are known to interact with dozens of other drugs and substances. Drug tests often show that patients are mixing them with other medications to elevate the drug effect, but instead, it results in various adverse reactions much more often. For example, opioids and benzodiazepines are two different kinds of medication that can cause severe interactions when taken together. They can cause opioid overdose symptoms and severe side effects which can even be fatal.
Opioids and Benzodiazepines Interactions
Benzodiazepines are prescribed to treat anxiety, muscle spasms, and seizures. Both benzodiazepines and opioids provide a relaxing and sedative effect by inducing relaxation in the central nervous system. When benzos and opioids are taken together, the risk of overdose increases. Users tend to take both of these medications together as the effect of pain relief is enhanced when combined with benzodiazepines. One of the most common risks associated with mixing opioids and benzodiazepines is increased sedation and unconsciousness. This can even cause users to slip into a coma. Both of these medicines depress breathing which can reduce the supply of oxygen to the brain. This can adversely affect the vital organs in the body as well as result in brain damage or even death.
The Interactions Of Opioids And Depressants
Depressants are prescribed for insomnia, anxiety, hypertension, and seizures. They include sedatives (Xanax and Valium), barbiturates (Phenobarbital and Butalbital), and tranquilizers (Klonopin). Opioids belong to a highly addictive set of drugs that can cause dependence and tolerance with prolonged use. When individuals develop a tolerance to them, they may take other substances to enhance the effect. However, when combined with depressants, the risk of overdose dramatically increases. The typical opioid addiction signs and symptoms worsen when it is combined with depressants. Risks associated with this kind of drug mixing include breathing problems, confusion, unconsciousness, and coma.
Opioids And Stimulants Interactions
Stimulants are a class of drugs that temporarily increase one’s alertness, wakefulness, and energy. According to a study of medical doctors from Florida, using opioid and stimulant drugs together may increase the risk of drug dependence and overdose. This happens because these two drug classifications have the potential to be abused and misused. Some of the stimulant medications include Ecstacy, Adderall, and Focalin.
Opioids And Hallucinogens Interactions
Hallucinogens are psychoactive agents which cause distortions in one’s perceptions, hallucinations, and changes in thoughts and consciousness. Combining opioids and hallucinogens can result in increased severity of adverse effects such as CNS depression which may require immediate medical care and attention. Some of the hallucinogenic drugs include shrooms, DMT, and LSD.
Opioids And Muscle Relaxers Interactions
Muscle relaxers are prescribed to treat muscle spasms, pain, and spasticity. They work in the brain and spinal cord to block or reduce the excessively stimulated nerve pathways. When muscle relaxant pain relievers and opioids are combined, it can increase the risk of overdose as well as the severity of side effects such as respiratory depression. Some of the muscle relaxant agents include Zanaflex, Baclofen, and Cyclobenzaprine.
Opioid Interactions With Other Substances
Individuals on pain-relieving treatment often mix it with other substances such as alcohol and marijuana to enhance the effect. This kind of mixing often results in undesirable and serious effects such as the increased risk of CNS depression, which can even prove to be fatal. It is recommended to seek resources such as addiction treatment for opioids if such behavior patterns were noticed.
Opioids and Alcohol
Mixing alcohol and opioid drugs can cause Serotonin Syndrome. This syndrome is characterized by an increase in the amount of serotonin in the body and causes confusion, increased heart rate, and agitation. This mix can also lead to severe effects such as seizures and tachycardia. Other effects of opioids and alcohol interaction include profound sedation, respiratory depression, coma, and death.
Opioids and Marijuana and CBD
Marijuana has been used for medicinal purposes for many years as an effective pain reliever. Similarly, CBD has also been legalized in many states to be used for pain relief. According to a clinical trial of medical doctors from the United States, Marijuana and opioids as well as CBD and opioids, when combined, may enhance pain relief properties but only when used in controlled doses for the short term. In the same study, it was reported that patients who use these opioid drugs and CBD properly under the care and intervention of a medical doctor may experience improved quality of life.
Managing Opioid Side Effects
The excessive use of any drug is not good for health in the long term. One must always consult a doctor before taking any prescription painkiller, especially those containing opioid substances. Natural laxatives such as chia seeds, leafy greens, and berries can be given by a doctor as an opioid induced constipation treatment in case of extreme opioid constipation. To relieve the symptoms of dry mouth, it is essential to remain hydrated by increasing the intake of water. If the medication is causing drowsiness, it should be taken during the nighttime, when the user does not have to partake in chores or other activities. In the case of abuse, one should consider resources such as enrolling in an addiction treatment program. This is considered the best step to overcome it. Treatment facilities provide a range of detox programs and further recovery therapies at reputable rehab.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Page Sources
- Ajo, R., Segura, A., Margarit, C., Ballester, P., Martínez, E., Ferrández, G., ... & Peiró, A. M. (2017). Erectile dysfunction in patients with chronic pain treated with opioids. Medicina Clínica (English Edition), 149(2), 49-54.
- Boom, M., Niesters, M., Sarton, E., Aarts, L., W Smith, T., & Dahan, A. (2012). Non-analgesic effects of opioids: opioid-induced respiratory depression. Current pharmaceutical design, 18(37), 5994-6004.
- Daoust, R., Paquet, J., Cournoyer, A., Piette, É., Morris, J., Lessard, J., ... & Chauny, J. M. (2020). Side effects from opioids used for acute pain after emergency department discharge. The American journal of emergency medicine, 38(4), 695-701.
- Fischer, M. A., & Jan, A. (2019). Medication-overuse headache.
- Freye, E., Baranowski, J., & Latasch, L. (2001). Dose-related Effects of Controlled Release Dihydrocodeine on Oro-Cecal Transit and Pupillary Light Reflex. Arzneimittelforschung, 51(01), 60-66.
- Katchman, A. N., McGroary, K. A., Kilborn, M. J., Kornick, C. A., Manfredi, P. L., Woosley, R. L., & Ebert, S. N. (2002). Influence of opioid agonists on cardiac humanether-a-go-go-related gene K+ currents. Journal of Pharmacology and Experimental Therapeutics, 303(2), 688-694.
- Kumar, L., Barker, C., & Emmanuel, A. (2014). Opioid-induced constipation: pathophysiology, clinical consequences, and management. Gastroenterology research and practice, 2014.
- Mallappallil, M., Sabu, J., Friedman, E. A., & Salifu, M. (2017). What do we know about opioids and the kidney?. International journal of molecular sciences, 18(1), 223.
- Mercadante, S., & Arcuri, E. (2005). Hyperalgesia and opioid switching. American Journal of Hospice and Palliative Medicine®, 22(4), 291-294.
- Ohishi, A., Chisaki, Y., Hira, D., Nagasawa, K., & Terada, T. (2015). Opioid analgesics increase incidence of somnolence and dizziness as adverse effects of pregabalin: a retrospective study. Journal of pharmaceutical health care and sciences, 1(1), 1-7.
- Ricardo Buenaventura, M., Rajive Adlaka, M., & Nalini Sehgal, M. (2008). Opioid complications and side effects. Pain physician, 11, S105-S120.
- Rogers, E., Mehta, S., Shengelia, R., & Reid, M. C. (2013). Four strategies for managing opioid-induced side effects in older adults. Clinical geriatrics, 21(4).
- Scott, L. J., & Perry, C. M. (2000). Tramadol. Drugs, 60(1), 139-176.
- Swegle, J. M., & Logemann, C. D. (2006). Management of common opioid-induced adverse effects. American family physician, 74(8), 1347-1354.
- Topaz, M., Seger, D. L., Lai, K., Wickner, P. G., Goss, F., Dhopeshwarkar, N., ... & Zhou, L. (2015). High override rate for opioid drug-allergy interaction alerts: current trends and recommendations for future. Studies in health technology and informatics, 216, 242.
- Walsh, T. D. (1990). Prevention of opioid side effects. Journal of pain and symptom management, 5(6), 362-367.
- Wei, Y. J. J., Zhu, Y., Liu, W., Bussing, R., & Winterstein, A. G. (2018). Prevalence of and factors associated with long-term concurrent use of stimulants and opioids among adults with attention-deficit/hyperactivity disorder. JAMA network open, 1(4), e181152-e181152.
- Zacny, J. P. (2001). Morphine responses in humans: a retrospective analysis of sex differences. Drug and alcohol dependence, 63(1), 23-28.

 Authored by
Authored by  Reviewed by
Reviewed by 

