Post-traumatic stress disorder (PTSD) is a mental health condition that affects people who have experienced intense life-threatening events, such as sexual assault, combat, terrorist incidents, or natural calamities.
The connection between substance abuse and trauma is well-established. Substance use disorders frequently co-occur in people with post-traumatic stress disorder. In fact, according to research published in the Journal of Clinical Psychology, PTSD and substance abuse are common, and people with post-traumatic stress are two to four times more likely to be diagnosed with an addiction.
Table Of Contents:
- What Is PTSD?
- What Are the Different Types?
- How Does It Manifest?
- What’s the Connection Between Trauma and Addiction?
- Why Are PTSD and Substance Abuse Connected?
- What Makes People Abuse Drugs?
- What Are the Dangers of Addiction In Military Personnel?
- How Are these Conditions Treated?
- What Therapies Are Used?

What is Post-Traumatic Stress Disorder?
It is not unusual for someone who has gone through a stressful event to feel on edge or have disturbing memories for a few weeks or months afterward. But if symptoms such as trouble sleeping and an inability to perform daily activities continue beyond a few months, it could be post-traumatic stress disorder.
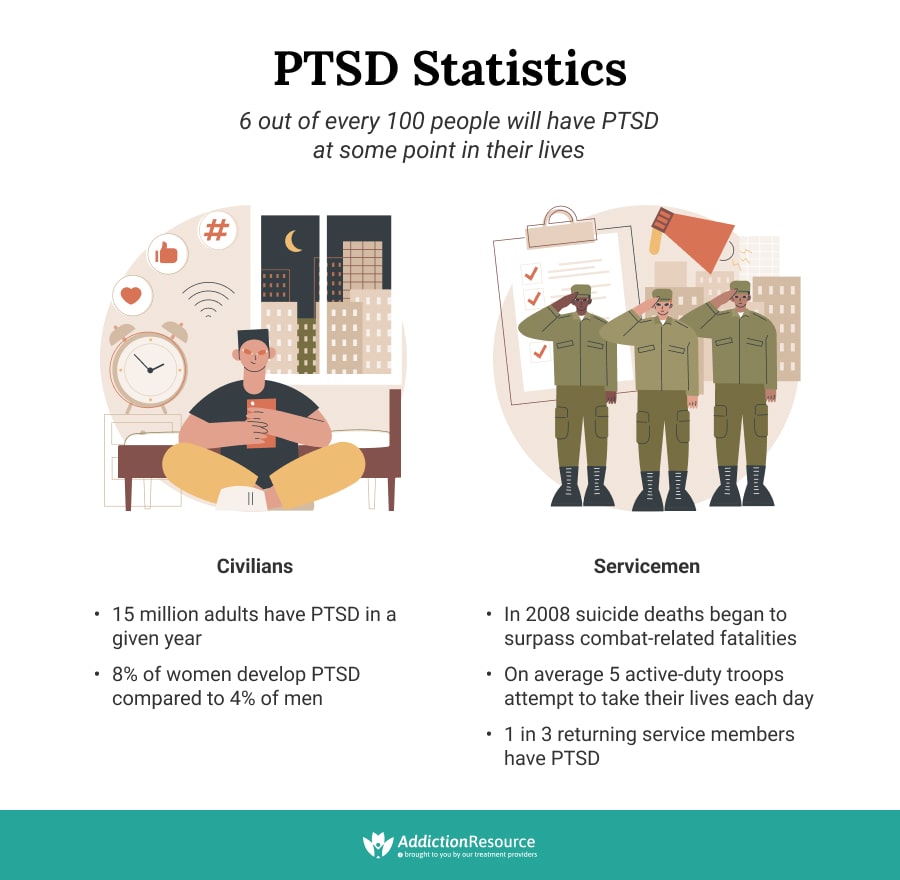
Anyone can develop this condition, which is a mental health condition and not a sign of weakness. People who have experienced prolonged trauma are more likely to develop different types of PTSD. For example, stress related to combat and sexual assault makes it more likely that the disorder will develop. In fact, 3 out of 10 people who have spent time in a war zone suffer from this condition.
It is noteworthy that post-traumatic stress disorder is twice as likely in women than men – 10 percent of women have PTSD at some point in their lifetime compared to 4 percent of men.
The condition affects an estimated 8 percent of Americans. It means almost 25 million Americans live with post-traumatic stress disorder at any given time.
PTSD causes are numerous, usually including trauma and stressful events. This disorder is more than just a bad mood or depression. It has both a psychological and physical component. People with post-traumatic stress often develop additional problems, such as memory difficulties, severe depression, or dependence on drugs or alcohol.
One study found that 65 percent of people experience a severe traumatic event at some point in their lives, enough to cause symptoms of PTSD, and more than 50 percent of these traumatized individuals go on to develop the condition.
The Common PTSD Causes Are:
- Natural disasters
- Terrorist attacks
- Serious accidents (car crashes)
- Sexual assault
- Domestic violence
- Childhood abuse
- Life-threatening illness
- Traumatic death/suicide by family member or friend
- Mugging or kidnapping
- Imprisonment or hostage situations
Anyone, regardless of gender, age, ethnicity, and occupation, can develop types of PTSD following exposure to a severely traumatic event. However, specific populations are more vulnerable than others. As mentioned, women are more likely to develop symptoms of post-traumatic stress than men. War veterans, firefighters, first responders, and police officers are high-risk groups based on their profession. Among the civilian population, victims of rape, domestic violence, and gang violence are at risk. This mental health condition is also seen in survivors of natural disasters, political confinement, ethnic imprisonment, or genocide.
Types of PTSD
Scientists have classified post-traumatic stress disorder into five main types based on the type of traumatic event and symptoms.
- Normal Stress Response. Among types of PTSD, this one occurs following a single discrete event during adulthood. Symptoms include having intense bad memories, feeling emotionally numb, and disconnecting from relationships. Recovery is usually possible in a few weeks with a debriefing, open discussions, and education on positive coping strategies.
- Acute Stress Disorder. It is relatively uncommon and occurs following a single life-threatening trauma. Symptoms include insomnia, suspicion, panic, confusion, dissociation, and inability to care for oneself. Treatment includes crisis intervention, removal from the scene, medications for anxiety and insomnia, and therapy.
- Uncomplicated PTSD. This type of post-traumatic stress disorder is relatively uncommon. It is typically associated with the persistent reliving of the traumatic event, avoidance of stimuli that provoke memories, emotional numbness, and heightened arousal. The treatment includes cognitive-behavioral therapy (CBT), group therapy, and pharmacological approaches.
- Comorbid PTSD. This is a common type, which includes co-occurring disorders like depression or a combination of PTSD and substance abuse. Treatment for dual diagnosis requires careful management of all coexisting conditions. Modalities include psychotherapy and medication-assisted therapy.
- Complex PTSD. This type of post-traumatic stress disorder occurs following exposure to prolonged stress such as sexual abuse during childhood or long-term deployment to a war zone. The signs include extreme emotional difficulties and antisocial behaviors such as aggression, alcohol and drug abuse, self-destruction, impulsiveness, and sexual misdemeanors. Treatment is usually prolonged and involves a structured therapy program delivered by specialists in post-traumatic stress disorder.
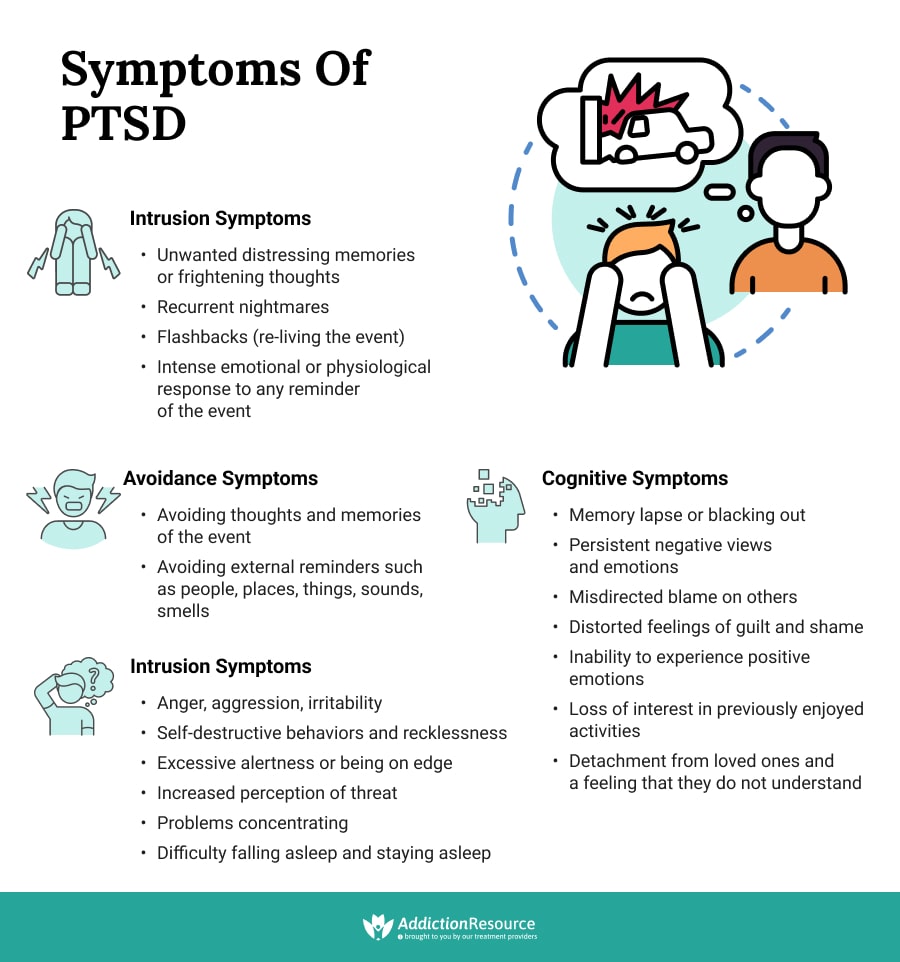
Symptoms of Post-Traumatic Stress Disorder
Different types of PTSD manifest as various physiological and psychological symptoms, ranging in severity from mild to debilitating.
Symptoms Are Divided Into Four Subgroups as Follows:
- Intrusion Symptoms
- Avoidance Symptoms
- Cognitive Symptoms
- Reactivity and Arousal Symptoms
Trauma and Addictions
Some people cannot cope with their post-traumatic stress disorder and begin to smoke too much, drink heavily, or use illicit drugs to deal with their symptoms. Due to a strong link between trauma and addictions, people struggling with post-traumatic stress are at high risk of developing problems with drugs and alcohol. Each of these conditions can make the symptoms of the other one worse. Much military personnel undergoing addiction treatment have coexisting PTSD. A dual diagnosis of addiction and PTSD is associated with many health and social problems.
Addiction and PTSD: Statistics and Facts
Many studies have shown a strong relationship between substance abuse and trauma in men and women in both military and civilian populations. One study found that people with PTSD were 14 times more likely to have a substance use disorder (SUD) than those without trauma-related stress. On the other hand, 30-60 percent of people seeking addiction treatment have PTSD.
Military Men and Women:
- 20 percent of war veterans suffer from addiction and PTSD at the same time.
- One-third of veterans seeking addiction treatment have post-traumatic stress disorder.
- 10 percent of soldiers who receive care at the Veterans Administration have alcohol or drug problems.
- PTSD and alcohol abuse is common in war veterans, especially binge drinking
- About 60 percent of veterans with this condition smoke compared to 30 percent without post-traumatic stress.
Non-Combat PTSD in Civilians:
- Nearly 90 percent of Americans are exposed to at least one traumatic event in their lifetime, and more than 10 percent develop composite event post-traumatic stress. Prevalence is highest following threat or injury to a loved one, witnessing dead bodies, witnessing a physical or sexual assault, or being the victim of sexual or physical assault.
- The lifetime prevalence of post-traumatic stress is just under 7 percent in the United States, with females showing a higher past-year prevalence (5.2 percent) than males (1.8 percent) and more than 36 percent of sufferers having severe disease.
- PTSD following rape is common, especially if it involves a stranger and the use of physical force or weapons
- Similar to trends in adults, PTSD in adolescents is higher in females (8 percent) compared to males (2.3 percent).
- Prevalence rates are high in countries with conflict, and causes of PTSD are determined by political and cultural factors, with physical violence being a common inciting event in countries such as South Africa and the death of a loved one in Europe and Japan.
- Up to 35 percent of patients diagnosed with cancer meet the criteria for full syndrome PTSD after completing treatment; some symptoms are present in up to 80 percent of patients with recurrent cancer.
The Chemistry of PTSD and Substance Abuse
According to the National Institute on Drug Abuse (NIDA), drug abuse may bring about symptoms of mental disorders, and mental disorders can lead to drug abuse. For example, people with PTSD may self-medicate and come to rely on drugs and alcohol for temporary relief from their symptoms. In addition, mental health disorders and addiction share common risk factors, such as genetic vulnerability and environmental triggers.

What happens in the brain and body of a person with PTSD? How to explain PTSD and alcohol or drug abuse connection? Alcohol, marijuana, benzodiazepines, and opioids are central nervous system suppressants. They enhance the activity of a neurotransmitter called GABA in the human brain. GABA is a natural tranquilizer that reduces fear and anxiety. Some illicit drugs increase the amount of dopamine, a chemical that makes us feel happy. Neurotransmitters called endorphins are released in the brain during traumatic events to cope with the stress and provide a sense of wellbeing. Once the traumatic event is over, there is endorphin withdrawal.
Drugs and alcohol can temporarily mimic the effects of these natural feel-good chemicals in the body. Individuals with PTSD start using alcohol and drugs to obtain these positive effects and relieve their symptoms. However, prolonged use of drugs and alcohol alters the structure of the neurons in the brain and causes permanent abnormalities in neurotransmission. Eventually, the person is unable to respond normally to these chemicals. With prolonged use, the individual becomes chemically dependent, requiring more and more drugs or alcohol to feel the same effects, eventually resulting in addiction.
Substance Abuse in Individuals with PTSD: A Coping Mechanism
The interplay between addiction and PTSD is complex and multifaceted. Studies show that in the majority of people, PTSD precedes substance abuse. So why do people with post-traumatic stress disorder start abusing drugs and alcohol? Experts believe it is a coping mechanism and a means of escape. High levels of stress make it more likely to turn to drugs or alcohol. For example, post-traumatic stress disorder can result in insomnia, and people with this condition may self-medicate with alcohol or drugs to try and fall asleep and stay asleep. Others may turn to illicit drugs or alcohol to numb terrible memories, avoid unpleasant emotions, or deal with a mood disorder.
Increased susceptibility also plays a role and puts some people with post-traumatic stress disorder at high risk of addiction. For instance, poor coping skills, genetics, biological vulnerability (family history of substance abuse), history of physical abuse or sexual assault, and prior exposure to combat or traumatic events can increase a person’s likelihood of developing an addiction to alcohol or drugs.
Such patients can become addicted to any mind-altering substance, but some addictions are more common than others. Here are some of the most commonly abused substances by people struggling with the aftereffects of trauma.
PTSD and Alcohol
In both male and female veterans and civilians, the most prevalent substances of abuse are tobacco and alcohol, probably because they are readily available and relatively inexpensive.

About 60 percent of veterans with PTSD smoke compared to 30 percent without post-traumatic stress disorder. According to the Veterans Administration, 60 to 80 percent of Vietnam vets who seek trauma treatment have problems with alcohol use. PTSD and alcohol abuse are the precursors to full-blown addiction. Studies show that comorbid alcohol use disorder and PTSD are highly prevalent in the U.S. veteran population. In civilians, PTSD and alcohol abuse often occur together and cause significant problems for the affected person. Trauma increases a person’s risk of drinking problems, and women are at greater risk than men. Victims of sexual abuse are at high risk of drug and alcohol problems. In fact, three out of four survivors of violent trauma report problems with alcohol.
Opiates
Opioids are highly addictive drugs frequently prescribed to veterans with chronic pain. Studies show that war veterans diagnosed with PTSD or other mental health conditions are more likely to receive an opioid prescription, higher doses of the medications, and early refills. Due to the link between trauma and addictions, people with PTSD can quickly become addicted to the euphoric escape that opiates offer, leading eventually to addiction. However, it makes the treatment even more complicated.
Many of the symptoms of opioid withdrawal, for example, agitation, hypervigilance, and easily startled, are similar to post-traumatic stress disorder symptoms.
Marijuana, Cocaine, and Amphetamines
Some people, after trauma, begin using marijuana as a self-treatment option. However, the drug is a psychoactive substance that leads to intoxication, euphoria, hallucinations, and sensorimotor dysfunction. Individuals trying to cope with trauma by relying on marijuana may become emotionally or chemically dependent on the drug without realizing the harm it can cause. Studies show that a diagnosis of PTSD significantly increases the risk of using marijuana. Among veterans seeking care at VA facilities for co-occurring substance use disorder and PTSD, cannabis use is the most common disorder. In 2014, nearly 23 percent of veterans with post-traumatic stress disorder and SUD had cannabis use disorder, up from 13 percent in 2002. Among other drugs, cocaine (15 percent), opioids (10-15 percent), and amphetamines (about 5 percent) are commonly abused by veterans.
Dangers of Addiction and PTSD in Military Men and Women
Military personnel struggling with the stress of deployments are at increased risk of PTSD and substance abuse. Addiction is a significant concern in the veteran community because it can have devastating consequences, especially when combined with illnesses and injuries from combat. Some of the dangers of addiction in military personnel returning home include:
Homelessness
The U.S. Department of Veterans Affairs reported a little under 40,000 homeless veterans in 2016, down from 76,000 in 2009. The majority of homeless vets are single males and suffer from alcohol or substance abuse and mental illness. Homelessness and drug abuse have a well-known connection, and about 70 percent of homeless vets have a substance use disorder. More than 10 percent of the homeless population in America are veterans with PTSD and alcohol abuse problems who end up on the street due to a lack of affordable housing, adequate income, and social support.
21% of veterans in substance use treatment were homeless in 2011.
Unemployment
Battling conditions such as PTSD and substance abuse with insufficient training for the civilian workforce, servicemen and women are at a disadvantage when competing for jobs, leading to unemployment. According to the Bureau of Labor Statistics, there were about 370,000 unemployed veterans in 2017, with nearly 60 percent of them in the 25 to 54 age group. The good news is that unemployment rates for veterans have been declining over the years.
Suicide
Research indicates a correlation between trauma, such as combat exposure or military sexual trauma, addiction and suicide risk. Studies suggest that PTSD is associated with suicidal behaviors. In fact, it is estimated that there is one suicide every 36 hours among members of the armed forces. Combat-related guilt for acts committed during a war is a predictor of suicide attempts. Moreover, in addition to suicidal ideation, combat veterans with depression are more likely to make fatal suicide attempts on their weapons training. Trauma treatment can help manage suicidal thoughts, but the key is ensuring that clinicians and mental health professionals screen carefully for these conditions in veterans.
Veterans make up 20% of national suicides, with 22 veterans dying each day by suicide.
Criminal Behavior
Veteran substance abuse has many devastating consequences. Poverty, homelessness, mental health conditions, and substance abuse all predispose an individual to criminal behavior. According to the Bureau of Justice Statistics, approximately 200,000 veterans are incarcerated in state and federal prisons, many for violent offenses. In addition, veterans with PTSD or traumatic brain injury are at an increased risk of death upon release from prison.
46% of veterans in federal prison were there for violation of drug laws, and 61% of all incarcerated veterans met the criteria for drug dependence.
Treatment of PTSD and Addiction
When PTSD and substance abuse are present together in a person, treatment is complicated because each condition fuels and magnifies the severity of the other. In addition, the withdrawal symptoms of many illicit drugs, such as sleep disturbance, irritability, detachment, and concentration problems, closely mimic the symptoms of PTSD.
Individuals with a dual diagnosis of PTSD and substance abuse have special needs and require intensive support from addiction experts, psychiatric specialists, as well as family, friends, and peers. Perhaps the biggest hurdle for many people is that they are in denial or are reluctant to reach out for help. Shame and guilt are common in people who have gone through a traumatic event. Addictive behaviors can add to these emotions and make it even more challenging to get appropriate treatment.

Dual diagnosis is difficult to treat because it is impossible to know where certain symptoms emanate from. For example, there is no way to tell whether a person’s depression is attributable to stress disorder or the drug. In addition, patients with a dual diagnosis are at high risk of suicide and require more intensive care.
It takes an integrated team of mental health professionals and addiction specialists to understand and treat addiction in people with co-occurring disorders. Individuals with these two conditions require comprehensive and customized treatment plans to address their unique needs. Not all drug rehabs can handle patients with a complicated dual diagnosis. Rehabilitation facilities with centralized resources to treat both conditions under one roof are the most successful in treating PTSD and substance abuse patients. Such facilities typically have healthcare professionals who have dealt extensively with individuals battling with both disorders.
Therapies Used in Treatment
The most crucial feature of dual diagnosis treatment is that both diagnoses should be addressed simultaneously. It ensures that all issues have been addressed once treatment is completed, and the person does not relapse to harmful behaviors or self-medication with drugs and alcohol. Highly trained teams of professionals provide parallel treatment for PTSD and substance abuse through several different treatment modalities
These Include:
- Cognitive-Behavioral Therapy. This treatment modality has proven efficacy in dual diagnosis treatment. The program typically consists of 16 sessions where the client unlearns preconceived notions and understands the relationship between feelings, thoughts, and behaviors. CBT is more than talk therapy. It requires the client’s active involvement in setting goals and following through with an eye on weekly progress.
- Eye Movement Desensitization and Reprocessing (EMDR). This type of therapy is very effective for individuals with trauma. Clients focus on and reprocess the traumatic event they experienced while tracking the oscillations of their eye movements. It helps reduce the terror associated with the event and changes how a person views the memory, thereby reducing the stress from the event and expediting recovery.
- Prolonged Exposure. PE therapy involves re-experiencing the traumatic event by recalling feelings, thoughts, and emotions. It addresses the avoidance symptoms and desensitizes the individual. This mechanism addresses the underlying symptoms that drive a person to drug use.
- Cognitive Processing Therapy (CPT). This type of therapy is especially effective in people with post-traumatic stress disorder. Incorporating elements of cognitive-behavioral therapy helps change negative thoughts associated with a traumatic event. The underlying principle of CPT is that negative emotions and behaviors are interconnected, and replacing them with positive ones is the key to recovery.
- 12-Step Programs. Alcoholism and trauma often go hand-in-hand. The 12-step approach has demonstrated efficacy in overcoming alcohol addiction. People who have experienced an intensely traumatic event often struggle with their spirituality and question their relationship with a higher power. When used in conjunction with other modalities, the 12-step format can be highly effective.
- Medication-Assisted Treatment. Anti-addiction medications, medications to make the withdrawal from drugs safer and easier, and medicines that control anxiety and depression are prescribed to assist people seeking help for PTSD and addiction.
- Alternative Therapies. People with dual diagnosis may benefit from alternative treatment modalities, such as relaxation techniques, guided imagery, breathing exercises, self-hypnosis, and yoga for addicts. These therapies help control the intense symptoms, which are the underlying forces leading to addiction.
Frequently Asked Questions
Can PTSD Cause Seizures?
Yes, PTSD can cause seizure-like symptoms. What patients actually experience is called pseudoseizure. Unlike an epileptic seizure, pseudoseizure is caused by psychological conditions and does not disrupt the nerve activity in the brain.
Is PTSD a Mood Disorder?
Post-traumatic stress disorder is a form of anxiety disorder and is not classified as a mood disorder. However, some patients may have comorbid PTSD and depression. In this case, the term “post-traumatic mood disorder” is used.
Does PTSD Cause Memory Loss?
Among common cognitive symptoms of PTSD are memory and concentration problems. Numerous studies have demonstrated the declarative memory dysfunction associated with PTSD. However, memory problems can also be caused by comorbidities like depression, addiction, or brain injury.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Page Sources
- Donley, M. S., Habib, L., Jovanovic, T., Kamkwalala, M. A., Evces, M., Egan, G., ... & Ressler, K. J. (2012). Civilian PTSD symptoms and risk for involvement in the criminal justice system. The journal of the American Academy of Psychiatry and the Law, 40(4), 522. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3752299/
- Alexander, D. A., & Klein, S. (2009). Kidnapping and hostage-taking: a review of effects, coping and resilience. Journal of the Royal Society of Medicine, 102(1), 16-21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2627800/
- Kilpatrick, D. G., Resnick, H. S., Milanak, M. E., Miller, M. W., Keyes, K. M., & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM‐IV and DSM‐5 criteria. Journal of traumatic stress, 26(5), 537-547. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4096796/
- NIMH, Post-Traumatic Stress Disorder (PTSD), https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd
- Davis, G. C., & Breslau, N. (1994). Post-traumatic stress disorder in victims of civilian trauma and criminal violence. Psychiatric Clinics of North America, 17(2), 289-299. https://pubmed.ncbi.nlm.nih.gov/7937360/
- Atwoli, L., Stein, D. J., Koenen, K. C., & McLaughlin, K. A. (2015). Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Current opinion in psychiatry, 28(4), 307. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4452282/
- National Cancer Institute, Cancer-Related Post-traumatic Stress (PDQ®)–Health Professional Version. https://www.cancer.gov/about-cancer/coping/survivorship/new-normal/ptsd-hp-pdq
- NIDA, Comorbidity: Substance Use Disorders and Other Mental Illnesses DrugFacts, 2018. https://www.drugabuse.gov/publications/drugfacts/comorbidity-substance-use-disorders-other-mental-illnesses
- Carter, A. C., Capone, C., & Eaton Short, E. (2011). Co-occurring posttraumatic stress disorder and alcohol use disorders in veteran populations. Journal of dual diagnosis, 7(4), 285-299. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3474251/
- SAMHSA, Twenty-one Percent of Veterans in Substance Abuse Treatment Were Homeless, 2014. https://www.samhsa.gov/data/sites/default/files/spot121-homeless-veterans-2014.pdf
- Wortzel, H. S., Blatchford, P., Conner, L., Adler, L. E., & Binswanger, I. A. (2012). Risk of death for veterans on release from prison. The journal of the American Academy of Psychiatry and the Law, 40(3), 348. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5262440/
- Huff, J. S., & Murr, N. (2021). Psychogenic Nonepileptic Seizures. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441871/
- Sher, L. (2005). The concept of post-traumatic mood disorder. Medical Hypotheses, 65(2), 205-210.https://pubmed.ncbi.nlm.nih.gov/15922089/

 Authored by
Authored by  Reviewed by
Reviewed by 