Oxycodone Side Effects: Can They Be Life-Threatening?

Oxycodone is a potent opioid medicine commonly used for moderate to severe pain management in cancer and certain chronic conditions. It is effective for around-the-clock pain treatment and should not be used on an as-needed basis. Its regular use causes different undesirable Oxycodone side effects and results in addiction and physical dependence. Learn about the typical OxyContin side effects, precautions, and recommended doses.
Table Of Contents:
Common Oxycodone Side Effects
Along with pain relief, Oxycodone (available under the brand of OxyContin) comes with undesirable health effects, which might differ according to the patient’s condition and medication dose and must be balanced for adequate pain management.
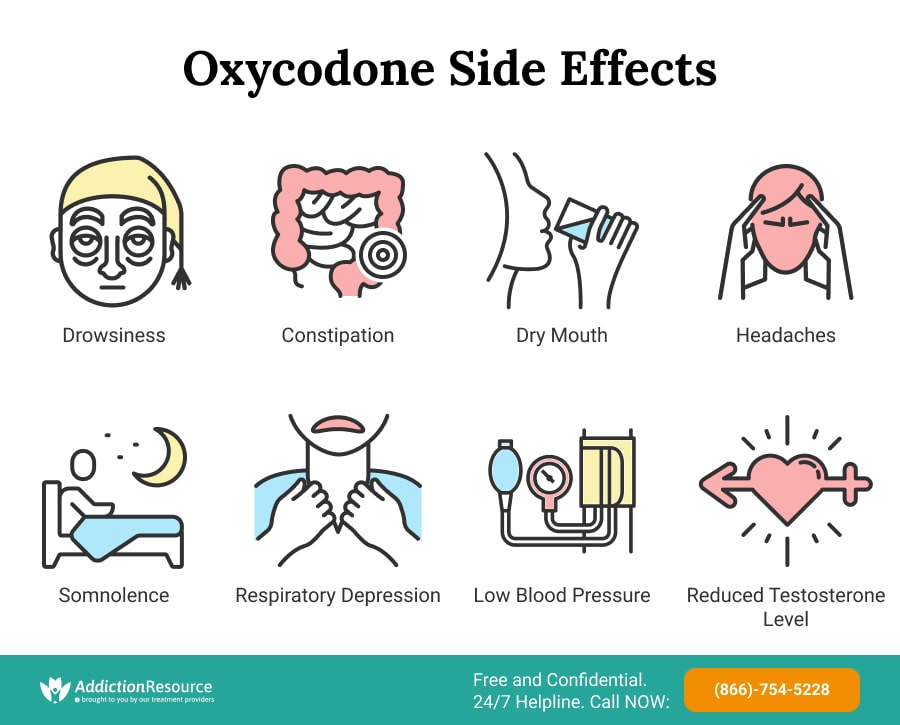
Following Are the Common Side Effects of Oxycodone:
- Drowsiness
- Nausea
- Vomiting
- Constipation
- Pruritus
- Dry mouth
- Headache
- Somnolence
Other undesirable health effects that are comparatively less common include sweating, flushing, mood changes, abdominal pain, depression, anxiety, decreased libido, breathing problems, and confusion.
Serious Adverse Reactions
The severity of the Oxycodone side effects is also dose-dependent and may lead to different health issues and death. People taking this medicine more than the recommended dose or for an extended period may experience complications with their mental and physical health.
Severe Oxycontin Side Effects Include:
- Oxycodone Addiction. Addiction is among the most severe side effects of Oxycodone. The habit-forming medicine can lead to increased drug tolerance, resulting in overdose and even fatality. Withdrawal symptoms, such as restlessness, lacrimation, sweating, mydriasis, and rhinorrhea, are observed when the opioid is discontinued.
- Respiratory depression. Severe and fatal respiratory depression can be caused even if this medication is used as per recommendation. Respiratory depression is more pronounced when this opioid is used in conjunction with benzodiazepines. This condition may also lead to respiratory arrest and even death if not treated on time. It is more likely to occur in elderly or debilitated patients since they may have changed pharmacokinetics than younger, healthier patients.
- Very low blood pressure. Using this opioid also causes severe hypotension, which includes syncope and orthostatic hypotension. This condition is more pronounced in patients using CNS depressants or who have low blood volume. It can also cause vasodilation in patients with a circulatory shock, leading to decreased blood pressure.
- Constipation. Oxycodone constipation is reported as another severe side effect in certain cases. The use of OxyContin with anticholinergic drugs increases the severity of Oxycodone constipation in the patients. Anaphylactic shock is also reported during the treatment with this opioid.
This medication is contraindicated in certain diseases, which are worsened with its use. For example, it may increase the frequency of seizures in patients with seizure disorders. Moreover, patients with significant chronic obstructive pulmonary disease and pre-existing respiratory depression are at increased risk of reduced respiratory drive, even at recommended dosages.
Long-Term Reactions
The primary long-term reaction of this opioid use is the development of physical dependence on the pain reliever. Similarly to Hydrocodone or any other opioid, this medication can become very addictive, and even recommended use can lead to abuse.

Chronic abuse can lead to OxyContin overdose and cause serious medical complications. The overdose symptoms include drowsiness, trouble breathing, cold skin, muscle weakness, and unconsciousness. If not given proper treatment timely, this medicine overdose can prove to be fatal.
Using this opioid for over a month also causes adrenal insufficiency. In addition, this drug also reduces testosterone levels in males by 50%, according to the Drug and Alcohol Dependence journal. Other long-term reactions observed in patients include dental issues, disturbed chemicals levels in the brain, reduced threshold for pain, and liver damage.
Oxycodone Warnings
OxyContin is a controlled substance and can only be acquired on a prescription of a registered medical professional. Before taking this drug, patients should tell their doctor the vital information regarding any health conditions they might be experiencing or any other medications that they are on since Oxycodone side effects may cause these conditions to worsen.
Following Are the Oxycodone Warnings Issued by Food and Drug Administration (FDA):
- The use of this opioid can render its user to addiction. Oxycodone effects can also lead to drug abuse and misuse if not appropriately controlled.
- Patients must swallow Oxycodone extended-release tablets whole and avoid chewing, breaking, or dissolving them. Licking or crushing the tablets may give too much of the drug rapidly and cause serious problems, including overdose and death.
- Pregnant women, immediately before labor, must not take this medicine when the use of other analgesics is more appropriate.
- Breastfeeding mothers must tell the required information to the medical professional before taking this medication. If used, breastfed infants need to be monitored for excess sedation and slow breathing.
- People who take this opioid should avoid driving or operating dangerous machinery as this drug may impair their mental or physical abilities.
- This drug is contraindicated in patients with gastrointestinal obstruction, acute or severe bronchial asthma, and respiratory depression.
- Using this drug with alcohol and other CNS depressants (anxiolytics) is also cautioned to avoid profound drowsiness, respiratory depression, coma, and death.
- Sudden discontinuation of this medication can result in severe withdrawal symptoms. The dose should be tapered off over some time.
- Certain drugs tend to decrease the analgesia produced by this pain reliever; hence, they need to be avoided. They include partial agonist (buprenorphine) and mixed antagonist/agonist (nalbuphine, pentazocine, and butorphanol).
Use in Pregnancy
Opioid analgesics mostly fall under category C; however, this medication is categorized as a B category drug, currently presenting no evidence of fetal harm and no data available in human studies. However, its use is still cautioned during pregnancy as it may cause embryo-fetal toxicity. Moreover, it can cross the placental barrier and cause neonatal respiratory depression. Therefore, this drug can only be used in gestation where the benefits outweigh its risks.

What’s more, prolonged use during pregnancy can cause Oxycodone effects in newborns. It can cause neonatal opioid withdrawal syndrome in newborns, which could be life-threatening and needs proper treatment. Signs and symptoms are hyperactivity, vomiting, diarrhea, high-pitched crying, and no weight gain.
Use During Lactation
During lactation, the use of OxyContin is not recommended. It is secreted in breast milk and will develop respiratory distress, CNS depression, and other potential ADRs in the breastfed infants. If the use of Oxycodone is advised to the nursing mother, then breastfeeding is not recommended for the neonates, and they should be switched to formula milk.
Avoiding Side Effects of Oxycodone
Oxycodone is a potent opioid analgesic prescribed for pain relief in certain severe and chronic health conditions. This medication, like other prescription opioids, has significant dangers associated with it. Both short- and long-term undesirable effects of this drug can impact an individual’s brain and body in a severe manner.
When taking a medication that can lead to overdose and fatality, following all the precautions is crucial.
By using the dose recommended by the doctor, patients can manage the severity of the OxyContin side effects and prevent life-threatening conditions. In case of overdose or misuse, Naloxone should be readily available to reverse the undesirable effects. If a patient becomes addicted to Oxycodone, treatment can be provided using various behavioral and pharmacological approaches. Certain drugs, such as naltrexone and buprenorphine, are used to manage prolonged withdrawal symptoms and maintain sobriety in patients.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Page Sources
- Medline Plus. Oxycodone. 2019. https://medlineplus.gov/druginfo/meds/a682132.html
- National Institute on Drug Abuse. Prescription Opioids DrugFacts. 2021. https://www.drugabuse.gov/publications/drugfacts/prescription-opioids
- National Drug Intelligence Center. OxyContin Fast Facts. https://www.justice.gov/archive/ndic/pubs6/6025/6025p.pdf
- Anastassopoulos, K. P., Chow, W., Tapia, C. I., Baik, R., Ackerman, S. J., Biondi, D., & Kim, M. S. (2012). Economic study on the impact of side effects in patients taking oxycodone controlled-release for noncancer pain. Journal of managed care pharmacy: JMCP, 18(8), 615–626. https://doi.org/10.18553/jmcp.2012.18.8.615
- Jones, J. D., Mogali, S., & Comer, S. D. (2012). Polydrug abuse: a review of opioid and benzodiazepine combination use. Drug and alcohol dependence, 125(1-2), 8–18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3454351/
- Li, T., Cunningham, J. L., Gilliam, W. P., Loukianova, L., Donegan, D. M., & Bancos, I. (2020). Prevalence of Opioid-Induced Adrenal Insufficiency in Patients Taking Chronic Opioids. The Journal of clinical endocrinology and metabolism, 105(10), dgaa499. https://pubmed.ncbi.nlm.nih.gov/32866966/
- Bawor, M., Bami, H., Dennis, B. B., Plater, C., Worster, A., Varenbut, M., ... & Samaan, Z. (2015). Testosterone suppression in opioid users: a systematic review and meta-analysis. Drug and alcohol dependence, 149, 1-9. https://www.sciencedirect.com/science/article/pii/S0376871615000733
- Yazdy, M. M., Desai, R. J., & Brogly, S. B. (2015). Prescription opioids in pregnancy and birth outcomes: a review of the literature. Journal of pediatric genetics, 4(02), 056-070. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4795985/
- Jonas, W. C. (2013). Oxycodone administered as postpartum pain relief is associated with maternal report of infant central nervous system depression in breastfed infants. BMJ Evidence-Based Medicine, 18(1), 40-41. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.940.641&rep=rep1&type=pdf

 Authored by
Authored by  Reviewed by
Reviewed by 



