
Opioid Use Disorder (OUD) involves a pattern of opioid use that leads to significant impairment or distress, characterized by the inability to control consumption despite adverse effects. The condition is driven by changes in brain chemistry, particularly in areas associated with reward and motivation, making it difficult to cease use even in the face of negative outcomes.
The main symptoms of OUD include intense cravings, tolerance, withdrawal symptoms, and a loss of control over opioid use. These signs lead to dangerous behaviors, including misuse of prescription opioids or illegal drugs like heroin.
The primary causes of OUD include genetic predisposition, chronic pain, mental health disorders, and a history of substance abuse. Environmental factors such as stress, trauma, and easy access to opioids also contribute significantly to its development. Prolonged use of opioids alters brain chemistry, making the individual more dependent on the substance.
Table Of Contents:
- What is Opioid Use Disorder?
- What are the Signs & Symptoms of Opioid Use Disorder?
- What are the Causes and Risk Factors of Opioid Use Disorder?
- What are the Side Effects of Opioid Use Disorder?
- How to Diagnose Opioid Use Disorder?
- How to Support A Loved One with Opioid Use Disorder?
- What are the Treatment Options for Opioid Use Disorder?
- What is Opioid Withdrawal?
- What are the Common Types of Opioid Use Disorders?

The risks associated with OUD are severe, including an increased risk of overdose, respiratory depression, and long-term cognitive impairment. Opioid misuse leads to significant social, financial, and legal problems, which complicate recovery efforts.
Treatment options for OUD include medication-assisted treatment (MAT), cognitive behavioral therapy (CBT), and support groups. MAT helps reduce cravings and withdrawal symptoms, while CBT addresses the underlying psychological aspects of addiction. With the right treatment plan, individuals manage their opioid addiction and work towards a healthier, opioid-free life.
What is Opioid Use Disorder?
Opioid use disorder (OUD) is defined as the chronic use of opioids that causes clinically significant distress or impairment, according to Dydyk AM, Jain NK, Gupta M., et al. 2024, titled “Opioid Use Disorder.” The DSM-5 describes OUD as a pattern of opioid use that leads to problems or distress, with at least 2 of the 11 criteria occurring within 12 months. The severity of the OUD is determined by the number of criteria met: mild (2 to 3 criteria), moderate (4 to 5 criteria), and severe (≥6 criteria), according to a study by Lu T, Whitley SD, Wiegand TJ, et al. 2024, titled “Treatment of Opioid Use Disorder.” This disorder affects individuals’ physical and mental health, leading to severe complications without appropriate intervention.
The treatment of OUD primarily involves Medication-Assisted Treatment (MAT). There are three medications approved by the FDA for the treatment of OUD: buprenorphine, methadone, and naltrexone. All three of these treatments have been demonstrated to be safe and effective, as mentioned by the Food and Drug Administration (FDA) in “Information about Medications for Opioid Use Disorder (MOUD).” These drugs reduce withdrawal symptoms, manage cravings, and prevent relapse by blocking the euphoric effects of opioids. The approach is paired with behavioral therapies to address the psychological aspects of addiction, making it an evidence-based standard for OUD management.
The ICD-10-CM codes for opioid use disorder (OUD) are in the category F11. The code you use depends on whether the patient is using, abusing, or dependent on opioids and any associated complications. F11.10, F11.21, and F11.99 were applied most frequently to patients who had clinical diagnoses of OUD (64%, 89%, and 79%, respectively). F11.20, F11.23, and F11.90 were applied to patients who had a diagnostic mix of OUD and chronic pain without OUD, according to a study by Osterhage KP, Hser YI, Mooney LJ, et al. 2024, titled “Identifying patients with opioid use disorder using International Classification of Diseases (ICD) codes: Challenges and opportunities.” The four clinics applied codes inconsistently. These codes are required in designing personalized treatment plans and enabling structured healthcare interventions for affected individuals.
What are Opioids?
“Opioids are a class of drugs used to reduce moderate to severe pain. Opioids can be made from the opium poppy plant or in the laboratory. Opioids block pain signals by binding to opioid receptors on nerve cells in the brain, spinal cord, gastrointestinal tract, and other organs in the body. Some opioids may also be used to treat cough and diarrhea. Opioids used for pain relief are usually safe when taken for a short time and as prescribed by a health care provider, but they can be highly addictive and, as a result, have often been misused or abused,” as defined by the National Cancer Institute.
The severity and dangers of opioids vary depending on their type and usage. Prescription opioids like oxycodone, hydrocodone, and morphine are used under medical supervision but lead to overdose if misused. Synthetic opioids such as fentanyl are significantly more potent and associated with a high risk of fatal overdose, especially when combined with other substances. Illicit opioids like heroin are commonly abused and carry severe health risks, including respiratory depression, infectious diseases from unsafe injection practices, and death.
The opioid crisis highlights the dangers of these substances, with misuse leading to widespread addiction, overdose deaths, and societal costs. More than 120,000 people die every year of opioid overdose, many of them with fentanyl, an analgesic drug that is 50–100 times more potent than heroin or morphine, according to the World Health Organization (WHO). Public health efforts aim to balance the legitimate medical uses of opioids with strategies to minimize their misuse and associated risks.
How are Opioids Consumed?
Opioids are consumed in various forms, depending on their purpose and whether they are being used medically or illicitly. Prescription opioids are commonly taken in IV when in the hospital setting and taken orally in the form of pills, capsules, or syrups otherwise. However, when opioids are misused, individuals crush pills to snort the powder, allowing the drug to be absorbed more quickly into the bloodstream for an immediate high. Some also dissolve the crushed powder and inject it intravenously using needles, a method that provides rapid effects but carries significant risks, including infection and overdose.
Illicit opioids like heroin are injected, snorted, or smoked, with each method altering the speed and intensity of the drug’s effects. Fentanyl, a highly potent synthetic opioid, is consumed unknowingly, as it is frequently mixed with other drugs. These diverse methods of consumption not only influence the effects of opioids but also amplify the potential dangers, including overdose, transmission of diseases through shared needles, and long-term health complications.
How Long Do Opioids Stay in Your System?
Opioids stay in your system for the duration it takes for approximately five half-lives of the drug to pass, effectively clearing it from the body, as described by Lötsch J et al., 2005, in the study titled “Pharmacokinetic–Pharmacodynamic Modeling of Opioids.” The exact timeline varies based on the specific opioid’s half-life, with short-acting opioids like heroin or codeine clearing faster than long-acting ones such as methadone or buprenorphine.
In urine, which is the most common testing method, opioids like morphine, codeine, and heroin are detectable for 1 to 3 days, according to the U.S. Food and Drug Administration 2017, titled “Drugs of Abuse Home Use Test.” while longer-acting opioids like methadone or buprenorphine remain for 5 to 12.5 days, according to Drugs.com in “Does methadone show up on a drug test?”
Compared to urine testing, blood testing has a shorter detection window for opiates. Codeine is detectable in the blood for up to 1 day, heroin for up to 6 hours, and morphine for up to 3 days, according to Healthline in “How Long Will Traces of Opiate Drugs and Medications Stay in Your Urine?” This makes blood tests useful for identifying recent drug use. Heroin is identifiable in saliva for up to 5 hours post-use, while morphine and codeine remain detectable for as long as 4 days, according to Healthline. In hair, opioids are detectable for up to 90 days, providing a long-term record of use, according to Testin.com in “Opioid Testing.”
Why are Opioids Addictive?
Opioids are addictive primarily due to their ability to activate the brain’s reward system. When opioids are used, they bind to specific receptors in the brain known as opioid receptors, according to the Mayo Clinic in “How opioid use disorder occurs.” These receptors are part of the body’s natural pain-relief system, but when opioids are introduced in larger quantities, they flood the brain with dopamine, a neurotransmitter associated with pleasure and reward. This surge creates feelings of euphoria, which encourages individuals to continue using the drug to experience that “high” again.
Over time, repeated use of opioids leads to changes in the brain’s neurochemistry, making it difficult for individuals to feel pleasure from anything other than the substance. This phenomenon is referred to as “tolerance,” where increasingly larger doses are needed to achieve the same effects, and “dependence,” where the body becomes reliant on the substance to function normally.
According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), Opioid Use Disorder (OUD) is diagnosed when there is a pattern of opioid use leading to clinically significant impairment or distress, manifested by at least two of the following within 12 months: strong cravings, inability to reduce use despite efforts, tolerance, withdrawal symptoms, and continued use despite negative consequences (e.g., social, legal, or physical harm). The disorder ranges from mild to severe, with severe cases significantly impairing daily functioning.
The addictive nature of opioids is due not only to their immediate effects on the brain’s reward circuits but also to the psychological components of addiction, according to the Substance Abuse and Mental Health Services Administration (SAMHSA)in a book titled “Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health.”
Genetic predisposition, environmental factors, and prior exposure to stressors contribute to an individual’s vulnerability to opioid addiction, as studied by Volkow ND, Blanco C., et al. 2021 in “The changing opioid crisis: development, challenges, and opportunities.” The brain’s neuroplasticity, its ability to change and adapt, as chronic opioid use leads to enduring alterations in how the brain processes reward and motivation, further cementing the cycle of addiction.
How Common is Opioid Use Disorder?
Opioid Use Disorder (OUD) is very common, affecting over 16 million people worldwide and over 2.1 million in the United States, according to a study by Dydyk AM, Jain NK, Gupta M., et al. 2024, titled “Opioid Use Disorder.” More than 120,000 deaths worldwide every year are attributed to opioids, as reported by Chang HY, Kharrazi H, et al. 2018, in “Healthcare costs and utilization associated with high-risk prescription opioid use: a retrospective cohort study.”
In 2022, an estimated 3.7% of U.S. adults (9,367,000) needed OUD treatment. Among these, 55.2% (5,167,000) received OUD treatment, and 25.1% (2,353,000) received medications for OUD. Most adults who needed OUD treatment either did not perceive that they needed it (42.7%) or received treatment that did not include medications for OUD (30.0%), according to a report by the Centers for Disease Control and Prevention (CDC) titled “Treatment for Opioid Use Disorder: Population Estimates — United States, 2022.”
Demographically, opioid use disorder disproportionately affects various populations, as studied by Vasilenko SA, Evans-Polce RJ, Lanza ST. et al. 2017, in “Age trends in rates of substance use disorders across ages 18-90: Differences by gender and race/ethnicity.” For instance, individuals between the ages of 18 and 44 years are most likely to experience OUD, with white Americans reporting the highest rates of opioid-related deaths. However, the epidemic also impacts racial and ethnic minorities, with rising overdose deaths among Black and Latino communities in recent years. Rural areas, in particular, have experienced heightened rates of opioid misuse and overdose deaths, a pattern linked to limited access to healthcare and addiction treatment resources.
The opioid epidemic is not only characterized by the high rates of addiction but also by its impact on overdose deaths. More than 120,000 people die every year of opioid overdose, many of them with fentanyl, an analgesic drug that is 50–100 times more potent than heroin or morphine, according to the World Health Organization (WHO). According to the CDC, synthetic opioids like fentanyl have been responsible for a significant portion of overdose deaths. In 2019, synthetic opioids contributed to 73% of opioid-related fatalities.
What is the Difference Between Opioid Use Disorder and Opioid Dependence?
The main difference between opioid use disorder (OUD) and opioid dependence is that opioid dependence is a subset of opioid use disorder, focusing on the physiological aspects of addiction, while OUD is more comprehensive, capturing both physical dependence and the broader patterns of problematic behavior associated with opioid use.
Opioid Use Disorder, as outlined by the DSM-5, includes a variety of behavioral and psychological symptoms related to opioid misuse, such as continued use despite negative consequences, unsuccessful attempts to reduce use, and cravings. It involves the problematic pattern of opioid use that leads to significant distress or impairment in a person’s life. OUD is categorized as mild, moderate, or severe based on the number of criteria met and includes both physical and psychological aspects of addiction.
Opioid dependence, on the other hand, was a term previously used in the DSM-IV to describe a physical state where the body becomes reliant on opioids. Dependence is marked by tolerance (the need for higher doses to achieve the same effect) and withdrawal symptoms when opioid use is reduced or stopped. This physical dependence is a component of OUD, but it does not encompass the full range of behaviors and psychological factors involved. In the DSM-5, opioid dependence was absorbed into the broader diagnosis of OUD, with a focus on both physical and psychological aspects.
What are the Signs & Symptoms of Opioid Use Disorder?
The signs and symptoms of opioid use disorder are intense cravings for opioids, inability to control or reduce opioid use, and developing tolerance, which requires higher doses to achieve the same effect. These signs indicate that an individual is struggling with opioid addiction. Intense cravings include both physical and psychological symptoms, severely affecting an individual’s ability to function in daily life.
The severity of opioid use disorder varies, but these symptoms collectively indicate a major disruption in physical health, mental well-being, and social functioning. For example, withdrawal symptoms such as anxiety, agitation, muscle pain, and nausea are severe and distressing, prompting individuals to continue using opioids to avoid them. Social consequences, such as strained relationships and neglect of responsibilities, further exacerbate the disorder, contributing to a downward spiral in an individual’s quality of life. The chronic and progressive nature of opioid addiction, if left untreated, results in overdose, long-term physical harm, and significant psychological distress.
These signs and symptoms of opioid use disorder are listed below:
- Intense cravings for opioids: Intense cravings are an overwhelming desire to use opioids, which leads individuals to seek out and use the drug even when they know it is harmful. These cravings are primarily psychological symptoms, causing the individual to become consumed by thoughts of obtaining and using opioids. The severity of these cravings makes it nearly impossible to focus on anything else, and they are one of the key drivers of continued opioid use despite negative consequences, according to a study by Kakko J et al. 2019, titled “Craving in Opioid Use Disorder: From Neurobiology to Clinical Practice.”
- Inability to control or reduce opioid use: The failure to stop or minimize opioid consumption despite the individual’s best intentions or attempts is another core sign of OUD. It is a psychological symptom rooted in addiction, where the person desires to quit but finds it extremely difficult due to the compulsive nature of the behavior, as mentioned in “DSM-5 Criteria for Diagnosis of Opioid Use Disorder.” This inability to control use leads to continued consumption, causing both short-term harm (e.g., risk of overdose) and long-term damage (e.g., chronic health problems). The severity of this symptom escalates over time, especially in the absence of treatment.
- Tolerance requiring higher doses to achieve the same effect: Tolerance occurs when an individual needs increasing amounts of opioids to achieve the same euphoric effects they once experienced with smaller doses. Tolerance is a physical symptom that indicates the body has adapted to the drug, and it reflects the growing dependence on opioids. Opioid-tolerant patients are those who have been using a daily dose for at least one week of 60 mg of morphine, 30 mg of oral oxycodone, 8 mg of oral hydromorphone, or an equivalent amount of another opioid, as explained by the Food and Drug Administration (FDA). The severity of this symptom is marked by a constant increase in dosage, which leads to dangerous levels of opioid consumption, significantly heightening the risk of overdose.
- Withdrawal symptoms when not using opioids: Withdrawal symptoms are physical and psychological reactions that occur when the body is deprived of opioids. These include anxiety, sweating, nausea, muscle aches, and irritability, among others, according to “Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings.” Withdrawal is a severe physical symptom that occurs because the body has become dependent on the substance, and it is both highly uncomfortable and dangerous. For many individuals, the fear of withdrawal is a major factor in their continued opioid use.
- Continued use despite harmful physical, psychological, or social consequences: Continued use of opioids is indicative of the deepening nature of addiction, where the individual continues to use opioids even though they are aware of the harm it is causing. The damage is physical (e.g., organ damage, overdose risk), psychological (e.g., anxiety, depression), or social (e.g., damaged relationships, loss of employment). This is a hallmark of addiction, reflecting both physical and psychological symptoms, and it leads to the deterioration of the individual’s well-being over time.
- Neglecting responsibilities at work, school, or home due to opioid use: Individuals suffering from OUD lack attention to important personal or professional duties as a result of opioid use. The individual neglects their job, schoolwork, or family obligations because obtaining and using opioids becomes their primary focus. This is a significant psychological symptom, indicating that the addiction has taken priority over important aspects of life, leading to strained relationships and diminished quality of life. The severity of this symptom results in job loss, academic failure, or family conflict, according to a study by Daley DC. et al. 2013, titled “Family and social aspects of substance use disorders and treatment.”
- Spending excessive time obtaining, using, or recovering from opioids: When individuals dedicate a disproportionate amount of time to procuring opioids, using them, or recovering from their effects, it is a sign of Opioid Use Disorder (OUD). This symptom indicates the extent to which opioid use consumes an individual’s life, leaving little room for other activities. It is primarily psychological, reflecting the obsession and compulsion associated with addiction, and leads to significant disruption in daily functioning and a decline in overall health.
- Loss of interest in previously enjoyed activities: When a person with opioid use disorder loses interest in activities they once found enjoyable, this reflects a condition known as anhedonia. This is a psychological symptom where the brain’s reward system becomes dulled due to opioid use, leading to reduced pleasure in normal activities. The severity of this symptom leads to complete social withdrawal, further isolating the individual and exacerbating the addiction. According to a study by Stull et al. 2022, titled “Anhedonia and Substance Use Disorders by Type, Severity, and With Mental Health Disorders,” individuals with opioid use disorder (OUD) are more likely to experience anhedonia compared to those with other substance use disorders. The study, which analyzed data from a nationally representative sample of 30,999 adults, found that OUD had the highest odds of anhedonia, with a 95% confidence interval (CI).
- Using opioids in dangerous situations, such as driving while impaired: Using opioids in hazardous conditions, like impaired driving, is a clear indication of the lack of judgment that comes with addiction. This is a behavioral symptom with both physical and psychological components, as it shows the individual’s impaired decision-making and risky behavior despite knowing the potential for harm. This symptom is severe as it endangers not only the individual but also others around them.
- Financial or legal issues related to opioid acquisition or use: Financial and legal problems occur when individuals with opioid use disorder engage in illegal activities, such as buying opioids on the black market, or when they exhaust their financial resources to support their addiction. This symptom includes both physical and psychological components, as the individual resort to desperate measures to obtain the drug, leading to arrest, legal consequences, and financial ruin. The severity of this symptom harshly affects an individual’s livelihood and personal well-being. People who use opioids have high rates of unemployment—as high as 87% in a ‘severely addicted’ population seeking methadone maintenance, as studied by Segest E., Mygind O., Bay H., et al. 1990, titled “The influence of prolonged stable methadone maintenance treatment on mortality and employment: An 8-year follow-up.”
- Social isolation or strained relationships due to opioid use: Opioid use causes individuals to withdraw from family, friends, and social circles because they prioritize obtaining and using the drug. This symptom is primarily psychological, reflecting the emotional and relational impact of addiction, and leads to estranged relationships, loneliness, and further exacerbation of the disorder. The severity of this symptom is high, as it isolates the person, leaving them with fewer resources for recovery, according to a study by Roe L et al. 2021, titled “Isolation, Solitude and Social Distancing for People Who Use Drugs: An Ethnographic Perspective.”
More About Opioids:
What are the Causes and Risk Factors of Opioid Use Disorder?
The causes of Opioid Use Disorder (OUD) include chronic pain management, the overprescription of opioids, and recreational use of opioids. These causes stem from a combination of biological, psychological, and environmental factors. These causes contribute to the development and escalation of opioid misuse and addiction. However, additional factors such as genetic predisposition, altered brain chemistry, and co-occurring mental health disorders also play significant roles.
The causes of Opioid Use Disorder are as follows:
- Chronic pain management: Many individuals initially use opioids for legitimate medical reasons, such as managing chronic pain. Long-term use of prescription opioids leads to physical dependence and, eventually, addiction. According to a study by Klimas J, Gorfinkel L, Fairbairn N, et al. 2019, titled “Strategies to identify patients risks of prescription opioid when initiating opioids for pain: a systematic review,” the incidence rate of OUD from prescribed opioids as 2.5%.
- Overprescription of opioids: The overprescription of opioids has been a significant driver of the opioid crisis, with excessive and prolonged prescriptions leading to misuse and dependency. A 2018 FDA analysis found that opioid analgesic dispensing in retail outpatient settings decreased by over 16% from the first half of 2017 to the first half of 2018. According to the Center for Disease Control and Prevention (CDC) in “About Prescription Opioids,” in 2023, nearly 8.6 million Americans 12 years and older reported misusing prescription opioids in the past year.
- Recreational use of opioids: Some individuals use opioids recreationally, starting with pills obtained from friends, family, or street sources. This non-medical use increases the risk of developing OUD, as individuals easily escalate their use and transition from casual consumption to addiction. Each year, approximately 14,000 Americans die from heroin overdoses, while 902,000 use heroin annually, and 6.25 million people have used heroin at some point in their lifetime, according to a report by the National Center for Drug Abuse Statistics (NCDAS).
- Genetic predisposition: Genetic factors significantly contribute to the risk of developing OUD. Heritability estimates for opioid use disorder (OUD) range from 23% to 54%, based on twin and family study by Tsuang MT et al. 1998, titled “Co-occurrence of abuse of different drugs in men: the role of drug-specific and shared vulnerabilities.”
- Altered brain chemistry: Opioids alter the brain’s reward system by increasing dopamine levels, which reinforces the pleasurable feelings associated with drug use. Over time, this leads to physical dependence and changes in brain function, making it more difficult for individuals to quit without intervention, according to a study, “Brain Dopaminergic Signaling in Opioid Use Disorders (OUD).”
- History of substance abuse: A history of substance abuse, including alcohol or illicit drugs, is a significant risk factor for developing OUD. Individuals with prior substance use disorders are more likely to misuse opioids, as they already have impaired judgment and coping mechanisms.
- Early exposure to opioids: Early exposure to opioids, especially during adolescence, increases the likelihood of developing OUD later in life. Studies show that adolescents who misuse prescription opioids are at a higher risk of opioid dependency in adulthood, according to a survey by Cerda M, Santaella J, et al. 2015, titled “Nonmedical prescription opioid use in Childhood and Early Adolescence Predicts Transitions to heroin use in young adulthood: a national study.”
- Co-occurring mental health disorders: Mental health disorders, such as depression, anxiety, and PTSD, are closely linked to the development of OUD. People with these conditions turn to opioids as a form of self-medication, increasing the risk of addiction. A population-based study in Alberta, Canada, by Marshall T et al. 2023, titled “Preexisting mental health disorders and risk of opioid use disorder in young people: A case-control study,” underscores the significant role of preexisting mental health conditions as risk factors for developing opioid use disorder (OUD). Individuals with anxiety disorders were 2.53 times more likely to develop OUD, while those with depressive disorders had 2.20 times greater odds.
- Social or environmental influences: Living in environments where drug use is prevalent or in social circles where opioid use is normalized increases the risk of OUD. Social factors, such as peer pressure and community drug availability, initiate and perpetuate opioid misuse. According to a study by Magnan S et al. 2017 titled “Social Determinants of Health 101 for Health Care: Five Plus Five,” Social determinants of health (SDoH) are responsible for 80% to 90% of health outcomes.
- Peer pressure: Peer influence is particularly strong among adolescents and young adults who are introduced to opioids by friends or social groups. Peer pressure leads individuals to experiment with opioids and, in some cases, progress to regular use and addiction.
- Lack of education about opioid risks: Many individuals are unaware of the risks associated with opioid use, including the potential for addiction. This lack of education leads to improper use, such as taking higher doses than prescribed or sharing prescription opioids, both of which increase the risk of addiction.
- Trauma or adverse childhood experiences: Trauma, such as physical, emotional, or sexual abuse or exposure to adverse childhood experiences (ACEs), significantly increases the risk of developing OUD. According to the study by Swedo EA and Sumner SA et al. 2020, titled “Adolescent Opioid Misuse Attributable to Adverse Childhood Experiences,” nearly 1 in 50 adolescents (1.9%) reported opioid misuse in the past 30 days. Among these, approximately 60% had experienced at least one adverse childhood experience (ACE), and 10.2% had experienced five or more ACEs. Alarmingly, over 70% of recent adolescent opioid misuse was directly attributable to ACEs.
- Economic hardship: Economic challenges, such as unemployment or poverty, increase the likelihood of opioid misuse. Financial strain drives individuals to seek opioids for stress relief or as a way to cope with despair, escalating the risk of addiction.
- Limited access to healthcare or mental health resources: Lack of access to adequate healthcare or mental health support makes it harder for individuals to address underlying issues contributing to opioid misuse. People without proper care turn to opioids for relief from physical or emotional pain, which increases the risk of OUD.
- Use of opioids to self-medicate for emotional or physical conditions: Many individuals use opioids to alleviate physical pain or emotional distress. This self-medication behavior leads to dependency as individuals seek out opioids to cope with chronic pain or mental health issues, perpetuating the cycle of addiction.
What are the Side Effects of Opioid Use Disorder?
The side effects of Opioid Use Disorder (OUD) are drowsiness, confusion, constipation, nausea, and respiratory depression, among others, with both physical and psychological implications that severely impact quality of life. These effects exacerbate social, financial, and legal challenges, creating a cycle of dependency and harm.
These effects of OUD are explained below:
- Drowsiness: OUD results in excessive fatigue and lethargy because opioids act on the central nervous system (CNS) to induce sedation. This impairment hampers concentration, reaction times, and daily productivity. Studies on opioid-induced sedation demonstrate its interference with both physical and cognitive functioning, according to a survey by Shaiova L. et al. 2005, titled “The management of opioid-related sedation.”
- Confusion: Cognitive impairment occurs as opioids affect neural pathways responsible for memory and decision-making, leading to disorientation and difficulty processing information. Chronic use exacerbates these effects, increasing the risk of accidents and poor judgment.
- Constipation: A common side effect of opioid use, constipation occurs as opioids bind to receptors in the gastrointestinal tract, reducing peristalsis and motility. Prolonged constipation results in severe complications such as fecal impaction or hemorrhoids.
- Nausea and Vomiting: Opioids trigger the chemoreceptor trigger zone (CTZ) in the brainstem, leading to nausea and vomiting. This effect is particularly pronounced in individuals with high opioid dosages or during the early phases of use.
- Slurred Speech: Opioids depress CNS activity, reducing coordination and motor control needed for clear articulation. This symptom coincides with sedation and impairs social communication.
- Impaired Judgment: The euphoric effects of opioids impair decision-making by altering brain regions responsible for rational thought and risk evaluation. This increases susceptibility to risky behaviors, accidents, and substance misuse escalation.
- Respiratory Depression: Opioids suppress the brainstem centers that regulate breathing, causing potentially fatal reductions in respiratory rate. Respiratory depression is the leading cause of death in opioid overdose cases.
- Anxiety and Irritability: Chronic opioid use dysregulates the brain’s reward system, leading to heightened stress responses and emotional instability, including irritability and anxiety during withdrawal. Withdrawal anxiety lasts between 5 and 14 days, according to Medical News Today in “Is there a link between opioids and anxiety?”
- Depression: Opioid-induced changes to brain chemistry, particularly in dopamine pathways, contribute to depressive symptoms over time. This is further supported by a study by researchers at the University of Queensland linking opioid misuse with a heightened risk of mood disorders.
- Increased Tolerance: Repeated opioid use necessitates progressively larger doses to achieve the same effects as receptors become less sensitive, increasing the risk of dependency and overdose.
- Physical Dependence: With prolonged use, the body adapts to opioids, making it difficult to function without them. Physical dependence is evidenced by withdrawal symptoms when the drug is discontinued.
- Withdrawal Symptoms: Abrupt cessation or reduction in opioid intake causes intense physical discomfort, including muscle pain, sweating, and cravings, driven by the body’s physiological dependence on the substance, according to Health Direct in “Opioid withdrawal symptoms.”
- Social Isolation: As opioid misuse intensifies, individuals prioritize substance use over relationships, leading to social withdrawal and estrangement from family and friends.
- Financial Difficulties: The financial burden of sustaining opioid addiction leads to economic strain, debt, or theft to fund continued use. Financial instability compounds the challenges of recovery.
- Risk of Overdose: Misusing opioids, especially at higher doses or in combination with other depressants, significantly increases the likelihood of overdose and fatal outcomes, as reported by CDC, 2021.
- Strained Relationships: The erratic behavior, secrecy, and conflicts associated with opioid misuse result in strained family dynamics and loss of trust.
- Legal Issues: Illicit opioid acquisition or possession leads to arrests, incarceration, and long-term legal consequences, creating additional barriers to recovery.
- Neglected Responsibilities: Opioid dependency disrupts daily life, causing individuals to neglect work, school, and personal obligations, further contributing to instability and isolation.
How to Diagnose Opioid Use Disorder?
To diagnose opioid use disorder (OUD), healthcare providers rely on criteria established in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Diagnosis involves evaluating a patient’s physical health, behavioral patterns, and substance use history. OUD is identified when an individual exhibits at least two of the 11 criteria within 12 months. These criteria include persistent cravings, unsuccessful attempts to reduce or stop opioid use, spending excessive time obtaining or using opioids, neglecting responsibilities, and experiencing social or interpersonal conflicts due to opioid use.
Healthcare providers also assess for signs of physical dependence, such as tolerance (needing larger doses for the same effect) and withdrawal symptoms when opioids are discontinued. Screening tools like the Clinical Opiate Withdrawal Scale (COWS) and the DSM-5 Severity Checklist are used to supplement diagnosis. Laboratory tests, including urine, blood, or hair analysis, are utilized to confirm recent opioid use, while interviews explore psychological and social impacts.
How to Support A Loved One with Opioid Use Disorder?
To support a loved one with opioid use disorder, it is important to approach the situation with compassion and understanding while avoiding judgment. Begin by creating a safe and non-confrontational space where they feel comfortable sharing their struggles. Encourage them to seek professional help, such as therapy, addiction treatment programs, or medication-assisted treatments like methadone or buprenorphine, which are proven to aid recovery. Offer to help them find resources, including local rehab centers or support groups like Narcotics Anonymous.
Educate yourself about opioid use disorder to better understand their challenges and avoid stigmatizing language. Be patient, as recovery is a long and non-linear process. Providing practical support, such as accompanying them to appointments or helping with daily tasks, also makes a significant difference. Setting boundaries to protect your own well-being while maintaining a supportive presence is important. If needed, consider family therapy or counseling to address the impact of OUD on the broader family dynamic.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
What are the Treatment Options for Opioid Use Disorder?
The treatment options for Opioid Use Disorder include medical detoxification, cognitive behavioral therapy (CBT), and medication-assisted treatment (MAT). These approaches work together to address the physical, psychological, and social dimensions of opioid addiction, helping individuals regain control and rebuild their lives. Treatment strategies vary depending on the severity of the disorder, individual preferences, and other co-occurring conditions. Integrated treatment approaches significantly improve recovery outcomes by up to 75%, with reduced relapse rates and improved social functioning, according to research by the CDC.
The treatment options for opioid use disorder are as follows:
Medical Detoxification
Medical detoxification involves safely managing withdrawal symptoms under medical supervision. The goal is to stabilize the patient while removing opioids from the system. Detoxification is the first step before starting long-term treatment. The advantages of detox include professional support and access to medications like methadone or buprenorphine to reduce withdrawal discomfort. According to SAMHSA, 68% of people who complete drug and alcohol detox programs report their treatment to be successful.
However, detox alone is not a cure for OUD; relapse rates are high without follow-up care. Recovery time ranges from 5 to 10 days, depending on the individual’s opioid use history and overall health. Studies, such as those by Polydorou, S., & Kleber, H. D. et al. 2008, titled “Detoxification of Opioids,” emphasize the importance of integrating detox with comprehensive addiction treatments.
Cognitive Behavioral Therapy (CBT)
CBT focuses on identifying and changing negative thought patterns and behaviors associated with opioid use. It helps individuals develop coping mechanisms to manage cravings and stress triggers effectively. This therapy is highly effective when combined with MAT and is supported by studies like McHugh RK, Hearon BA, and Otto MW. et al. 2010, titled “Cognitive behavioral therapy for substance use disorders,” which highlights its role in reducing relapse rates, and more than 80% of participants were found to abstain from opioids at week 12. CBT involves weekly sessions over several months. Its advantage lies in its flexibility and adaptability, but it requires commitment and time to see sustained benefits.
Medication-Assisted Treatment (MAT)
MAT combines FDA-approved medications with behavioral therapies to treat OUD. Common medications include methadone, buprenorphine, and naltrexone, which help reduce cravings and block the euphoric effects of opioids. Methadone and buprenorphine are used for maintenance therapy, while naltrexone is ideal for preventing relapse after detox. While MAT is a long-term commitment, its advantages include improving retention in treatment and lowering the risk of overdose. However, concerns about dependency on maintenance medications and stigma are challenges.
According to a study by Connery HS et al. 2015, titled “Medication-Assisted Treatment of Opioid Use Disorder Review of the Evidence and Future Directions,” Methadone is considered to be the gold standard for the treatment of opioid use disorder, with research supporting its efficacy in keeping individuals opioid-free at rates as high as 60%.
Support Groups
Support groups like Narcotics Anonymous (NA) offer a community-based approach to recovery. These groups provide peer support, fostering accountability and shared experiences in a non-judgmental setting. While support groups are not a standalone treatment, they are an effective supplement to other therapies. The recovery process is ongoing, with no fixed timeline. Advantages include emotional support and reduced isolation, but the effectiveness depends on the individual’s level of participation. A Lancet journal estimates that only 5-8% of people who attend AA successfully maintain abstinence.
Inpatient Treatment
Inpatient treatment provides a structured environment with 24/7 medical and emotional support. Programs last 30–90 days and include a combination of detox, therapy, and skill-building workshops. Inpatient treatment is especially effective for individuals with severe OUD or co-occurring disorders. Advantages include intensive care and reduced exposure to triggers, but the high cost and time commitment are drawbacks.
12-Step Programs
Modeled after Alcoholics Anonymous, 12-step programs focus on spiritual and behavioral transformation through structured steps. These programs emphasize surrendering to a higher power, making amends, and fostering community support. Individuals who participate in support 12-step programs reduce their chance of relapse anywhere from 7% to 25%, according to a study by Tracy K Wallace SP. et al. 2016, titled “Benefits of peer support groups in the treatment of addiction.” The recovery process is ongoing and requires active participation. The advantage of accessibility and peer connection contrasts with criticisms of its spiritual focus, which does not align with everyone’s beliefs.
What is Opioid Withdrawal?
Opioid withdrawal is a physiological and psychological response that occurs when someone who has developed a dependence on opioids abruptly stops or significantly reduces their use. This condition arises because prolonged opioid use alters brain chemistry, particularly in pathways involving dopamine and endorphins, leading to physical reliance. Symptoms of withdrawal begin within hours to days of the last opioid dose, depending on the substance used and its half-life.
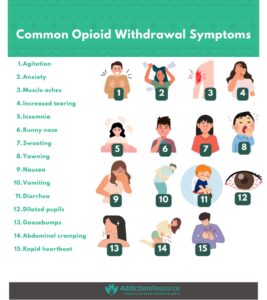
Withdrawal symptoms are divided into early and late phases. Early symptoms include agitation, anxiety, muscle aches, increased tearing, insomnia, and sweating. Later symptoms are more intense and include abdominal cramping, diarrhea, dilated pupils, nausea, vomiting, and rapid heart rate. While opioid withdrawal is rarely life-threatening, it is profoundly uncomfortable, driving many individuals back to substance use to avoid these effects.
Research highlights the complexity of opioid withdrawal. Studies like those by Kosten TR, George TP. et al. 2002, titled “The neurobiology of opioid dependence: implications for treatment,” emphasize the interplay of physical and psychological factors during withdrawal, underscoring the need for comprehensive treatment strategies. Withdrawal severity varies depending on the duration of opioid use, dosage, and individual health factors, including co-occurring mental health conditions. Treatments involve medications like methadone, buprenorphine, or clonidine, alongside supportive care, to alleviate symptoms and facilitate recovery.
What are Opioid Withdrawal Symptoms?
Some common opioid withdrawal symptoms are listed below:
- Agitation
- Anxiety
- Muscle aches
- Increased tearing
- Insomnia
- Runny nose
- Sweating
- Yawning
- Nausea
- Vomiting
- Diarrhea
- Dilated pupils
- Goosebumps
- Abdominal cramping
- Rapid heartbeat
What are the Common Types of Opioid Use Disorders?
Opioid Use Disorder (OUD) is categorized into different types based on the specific opioids involved and the severity of the addiction. The most common types of opioid use disorders include heroin use disorder, prescription opioid use disorder, and synthetic opioid use disorder. Heroin use disorder is characterized by the misuse of illicit heroin, leading to dependency and a high risk of overdose. Prescription opioid use disorder arises from the misuse of legally prescribed opioids such as oxycodone, hydrocodone, or morphine, commonly used for pain management but abused for their euphoric effects. Synthetic opioid use disorder involves the abuse of synthetic opioids like fentanyl, which are highly potent and carry an increased risk of fatal overdose.
These disorders share similar features, including physical dependence, tolerance, and withdrawal symptoms, but differ in the type of substance used and the context in which it is consumed. The risk factors and treatment strategies vary depending on the type of opioids involved, with heroin and synthetic opioids presenting more immediate and severe health risks due to their potency. Treatment approaches include medication-assisted treatment (MAT), counseling, and behavioral therapies, but they need to be tailored to the specific opioids involved to address the unique challenges of each type of OUD effectively.
What Types of Opioids Are the Most Common?
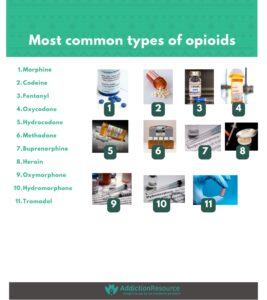
The most common types of opioids include morphine, codeine, fentanyl, oxycodone, and hydrocodone. These opioids are widely prescribed for pain management, though they are also misused, leading to opioid use disorder. Fentanyl and heroin are particularly potent and associated with the highest risk of overdose, while oxycodone and hydrocodone are frequently prescribed but also commonly abused. Other opioids like methadone and buprenorphine are used in treatment settings, but misuse of these medications also poses significant risks.
The most common types of opioids are as follows:
- Morphine: Morphine is a natural opioid used to manage severe pain, especially in post-surgical or cancer-related cases. It binds to opioid receptors in the brain and spinal cord to block pain signals. Morphine prescriptions at emergency department discharges declined by 23.2% from 2006–2007 to 2016–2017. National Health Statistics Report, 2020, titled “Trends in Opioids Prescribed at Discharge From Emergency Departments Among Adults: United States, 2006–2017.”
- Codeine: Codeine is used for mild to moderate pain and cough suppression. It is less potent than morphine and metabolizes into morphine in the liver. Codeine prescriptions decreased from 3.7% to 2.9% over the past decade. University of California San Francisco, 2020, titled “Trends in opioid prescribing and use in the United States: A retrospective cohort study of national health data.”
- Fentanyl: Fentanyl is a synthetic opioid 50–100 times more potent than morphine, used for severe pain management. Illicit fentanyl is a major contributor to overdose deaths. In 2022, approximately 73,838 overdose deaths involved fentanyl. Statistica, 2022, titled “Fentanyl overdose deaths U.S. 1999-2022.”
- Oxycodone: Oxycodone, used for moderate to severe pain, is a key contributor to the opioid crisis. About 1 million people reported nonmedical use of OxyContin in the U.S., with high school seniors also misusing it. National Household Survey on Drug Abuse, titled “Monitoring the Future: National Survey Results on Drug Use, 1975-2020.”
- Hydrocodone: Hydrocodone is the most prescribed opioid in the U.S. for moderate to severe pain. Misuse is widespread, and in 2022, 36.5 million people used hydrocodone products, with 10.2% misusing them. Substance Abuse and Mental Health Services Administration, 2022, titled “National Survey on Drug Use and Health: Detailed Tables.”
- Methadone: Methadone is used for opioid addiction treatment and chronic pain. It reduces cravings without causing euphoria. Methadone overdose deaths decreased by 1.3% from January 2019 to August 2021. Jones CM et al. 2022, titled “Methadone-Involved Overdose Deaths in the US Before and After Federal Policy Changes Expanding Take-Home Methadone Doses From Opioid Treatment Programs.”
- Buprenorphine: Buprenorphine is used in medication-assisted treatment for opioid addiction. It helps reduce cravings and withdrawal symptoms. The national dispensing rate for buprenorphine in 2023 was 4.7 prescriptions per 100 people. Centers for Disease Control and Prevention, 2023, titled “Buprenorphine Dispensing Rate Maps.” However, significant state-level variations were observed. Han B, Jones CM, et al. 2021, titled “Trends in and Characteristics of Buprenorphine Misuse Among Adults in the US.”
- Heroin: Heroin, an illegal opioid derived from morphine, is highly addictive and a leading cause of overdose deaths. In 2021, about 0.4% of U.S. individuals aged 12 or older reported heroin use. National Institute on Drug Abuse, 2021, titled “What is the scope of heroin use in the United States?”
- Oxymorphone: Oxymorphone is used for severe pain, with a rapid onset of action. Misuse is a concern, with 89 reported exposures in 2020. American Association of Poison Control Centers, 2020, titled “Annual Report of the American Association of Poison Control Centers National Poison Data System.” A study by Rauck R, Ma T, Adieh H, Kerwin R, et al. (2009), titled “Conversion and titration from oxycodone to oxymorphone extended-release in patients with chronic low back pain,” found higher success rates in switching from oxycodone to oxymorphone in chronic pain patients.
- Hydromorphone: Hydromorphone, 8 times stronger than morphine, is used for severe pain. Misuse is common, with approximately 102,000 individuals misusing hydromorphone products. Substance Abuse and Mental Health Services Administration, 2022, titled “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health.”
- Tramadol: Tramadol is a synthetic opioid used for moderate pain relief. Although less addictive, its misuse has increased. In 2022, there were 12.2 million tramadol prescriptions, and 9.4% of users misused it. Statistica, 2022, titled “Number of tramadol prescriptions in the U.S. from 2004 to 2022.”
What Opioids Are the Most Potent?
The most potent opioids include fentanyl, carfentanil, and methadone, among others.
Fentanyl is an extremely potent synthetic opioid, approximately 50 to 100 times stronger than morphine. It is used medically for severe pain, such as in cancer patients, but illicit fentanyl is a leading cause of overdose deaths. According to the Centers for Disease Control and Prevention (CDC), fentanyl is responsible for a significant portion of opioid overdose deaths in the U.S. and is commonly mixed with other drugs like heroin or cocaine, heightening the risk of fatal overdose.
Carfentanil, a fentanyl analog, is even more potent, around 100 times stronger than fentanyl and 1,000 times more potent than morphine. It is not intended for human consumption and is used as a tranquilizer for large animals like elephants. Its potency makes it highly dangerous, as even a small amount causes fatal respiratory depression.
Methadone, while used for treating opioid addiction, is also a potent opioid, particularly in the form of medication-assisted treatment (MAT). It is longer-lasting than many other opioids and effectively reduces cravings and withdrawal symptoms. However, due to its potency, it also poses a risk of overdose, especially if misused.
Other potent opioids include hydromorphone (which is approximately 8 times stronger than morphine) and oxymorphone (a powerful semi-synthetic opioid used for severe pain).
Can You Die from Opioid Overdose?
Yes, you can die from opioid overdose. When someone overdoses on opioids, the primary risk is respiratory depression, where breathing slows down or stops entirely, leading to a lack of oxygen in the body. This causes brain damage, organ failure, and death if not treated immediately. Fentanyl, a highly potent synthetic opioid, has significantly increased the risk of overdose deaths in recent years, especially when mixed with other substances such as heroin or cocaine, according to the National Institute on Drug Abuse (NIDA).
The Centers for Disease Control and Prevention (CDC) reports that opioid overdose deaths have risen dramatically, with synthetic opioids, particularly fentanyl, contributing to most of these deaths. In 2022 alone, more than 120,000 overdose deaths involved synthetic opioids like fentanyl.
However, with prompt administration of naloxone (Narcan), a medication that rapidly reverses opioid overdose symptoms, fatalities are prevented. Immediate medical attention is important, and naloxone is a life-saving tool in emergencies.
Who is at Risk of Opioid Use Disorder?
Individuals at risk of opioid use disorder (OUD) include those with a history of substance abuse, chronic pain, or mental health disorders, as well as those under high stress or experiencing emotional trauma. People who are prescribed opioids for pain management, especially in long-term or high-dose regimens, are at heightened risk of developing OUD. Other at-risk groups include medical professionals, who are more likely to misuse opioids due to easy access. According to the National Institute on Drug Abuse (NIDA), individuals with a family history of substance use disorders or who are living in environments where drug use is common are also more vulnerable to developing opioid addiction.
Are There Specific Support Groups for Opioid Use Disorder?
Yes, there are specific support groups for opioid use disorder. Groups such as Narcotics Anonymous (NA) and SMART Recovery provide peer support for individuals in recovery from opioid addiction. These groups offer structured environments where individuals share experiences, receive emotional support, and gain strategies for managing cravings. Support groups help maintain long-term recovery by fostering a sense of community and reducing isolation, which is common among those with substance use disorders.
Is Opioid Use Disorder a Disease?
Yes, opioid use disorder (OUD) is considered a chronic brain disease. It is characterized by the compulsive use of opioids despite the harmful consequences. This disorder alters the brain’s neurochemical processes, particularly those involved in reward and pleasure pathways. Over time, the brain becomes dependent on opioids, and individuals require increasingly higher doses to achieve the same effect, leading to addiction. The American Society of Addiction Medicine (ASAM) recognizes OUD as a medical condition, emphasizing that it involves changes in brain function and chemistry that affect behavior, decision-making, and emotional regulation.
What Impact Does Opioid Use Disorder Have on Pregnant Women and Their Newborns?
Opioid use disorder (OUD) has a significant impact on pregnant women and their newborns. For pregnant women, opioid use increases the risk of complications such as preterm labor, miscarriage, and placental abruption. Neonatal abstinence syndrome (NAS), a condition in which newborns experience withdrawal symptoms from opioids, is a major concern. NAS causes symptoms such as irritability, feeding difficulties, seizures, and poor weight gain. According to the Centers for Disease Control and Prevention (CDC), the incidence of NAS has increased significantly in recent years. From 2021 to 2022, the rate of hospital visits of male newborns with NAS increased 19% (6.4 to 7.7 per 1,000 live births), while the rate for female newborns increased 21% (5.6 to 6.9 per 1,000 live births). Effective treatment and prenatal care are important to minimize risks for both the mother and baby.
What Are Healthier Alternatives to Opioids for Pain Management?
Healthier alternatives to opioids for pain management include non-opioid medications, physical therapy, and cognitive behavioral therapy (CBT). Non-opioid medications like acetaminophen, ibuprofen, and topical treatments are effective for many types of pain without the risk of addiction. Physical therapy focuses on exercises and techniques to improve mobility and reduce pain, helping people avoid the need for painkillers. Cognitive behavioral therapy helps individuals manage pain by altering their thoughts and behaviors related to pain perception. The National Institutes of Health (NIH) suggests that these alternatives are safer and more effective in the long term for managing both acute and chronic pain.
What Are Opioids’ Effects on Brain Chemistry?
Opioids affect brain chemistry by binding to opioid receptors in the brain, spinal cord, and other areas of the central nervous system. These receptors are part of the brain’s reward system and are involved in pain relief and pleasure. When opioids activate these receptors, they trigger the release of dopamine, a neurotransmitter that plays a role in feelings of joy and reward. Over time, the brain becomes less responsive to natural dopamine and more reliant on opioids, leading to tolerance, dependence, and addiction. This alteration in brain chemistry is a key factor in the development of opioid use disorder, as the brain’s reward system becomes hijacked by the substance.
What Is the Prognosis of Opioid Use Disorder?
The prognosis for opioid use disorder (OUD) varies depending on the individual and the treatment they receive. With early intervention, appropriate treatment, and long-term support, many individuals recover and lead healthy, fulfilling lives. However, without treatment, OUD leads to serious complications such as overdose, chronic health conditions, and significant social and psychological problems. Medication-assisted treatment (MAT), therapy, and support groups have been shown to improve recovery rates and reduce relapse. The National Institute on Drug Abuse (NIDA) reports that with a combination of treatment approaches, recovery from OUD is possible, but it requires ongoing commitment and support.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
Find Drug Rehabilitation Centers Near You Anywhere In the US
Addiction Resource team has compiled an extensive list of the top drug rehabilitation facilities around the country. Use our locator tool to find the best centers near you.







 FindTreatment.gov
FindTreatment.gov