
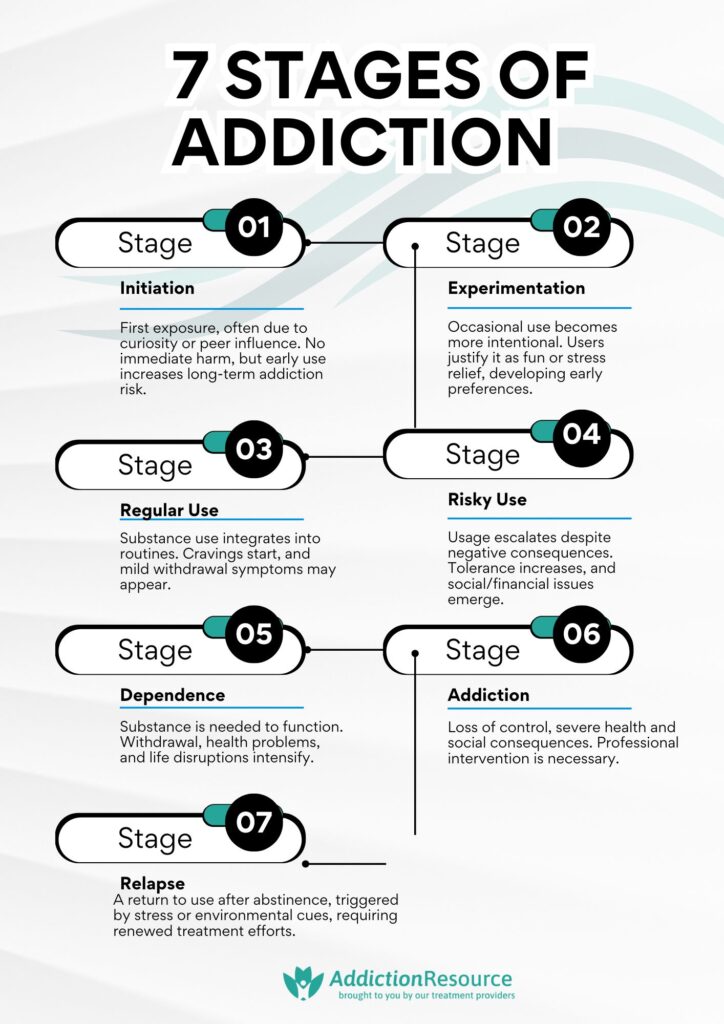
The Stages of Addiction follow a predictable pattern, beginning with initial exposure and potentially culminating in addiction and relapse. Each stage represents an increasing level of use and dependence, making early intervention required. Research from the National Institute on Drug Abuse (NIDA) suggests that recognizing warning signs early significantly reduces long-term addiction risks.
Initiation marks the first exposure to a substance, usually influenced by curiosity, peer pressure, or environmental factors. Adolescents are particularly vulnerable, as early drug use alters brain development, increasing the likelihood of addiction later in life (NIDA, 2020). At this stage, there are no significant negative effects, and use is experimental rather than habitual.
Experimentation follows initiation, where individuals begin using substances more deliberately in social settings. Though use remains occasional, patterns start forming, reinforcing the idea of substance use as a coping mechanism. The Journal of Adolescent Health reports that experimentation during adolescence is a strong predictor of future substance use disorders, especially when linked to emotional stress or trauma.
Regular use develops when substance consumption becomes more structured and frequent, occurring at specific times, such as weekends or after stressful events. Individuals experience mild withdrawal symptoms or increased tolerance. Regular use alters neural pathways, making individuals more prone to dependence and compulsive behaviors.
Risky use represents a significant escalation, where individuals continue using substances despite negative consequences such as declining health, relationship conflicts, or legal trouble. At this stage, substance use interferes with responsibilities and decision-making. The National Center for Biotechnology Information (NCBI) notes that risky use is strongly associated with reduced impulse control and an increased likelihood of developing substance dependence.
Dependence is characterized by a compulsive need to use substances to function normally. Withdrawal symptoms become more severe, leading to emotional instability and increased cravings. According to a study by the United Nations Office on Drugs and Crime, prolonged substance dependence results in cognitive impairments, making cessation increasingly difficult without medical intervention and structured treatment programs.
Addiction is the most severe stage, where substance use becomes uncontrollable and dominates all aspects of life. Physical and psychological deterioration intensifies, leading to financial ruin, legal issues, and social isolation. Even after achieving sobriety, relapse remains a significant risk. The NIDA reports that relapse rates for addiction range from 40% to 60%, comparable to other chronic diseases such as hypertension and diabetes.
1. Initiation
Initiation is the first stage in the progression of addiction, characterized by the initial exposure to a drug or addictive behavior. This stage occurs in adolescence or early adulthood and is influenced by peer pressure, curiosity, or environmental factors. The frequency of use at this stage is experimental or occasional, with no established pattern.
Individuals in the initiation stage do not experience any immediate adverse effects and perceive the substance as harmless or even enjoyable. However, even at this stage, psychological factors such as sensation-seeking behavior or underlying mental health conditions play a role. Physically, there are little to no immediate negative consequences, but early exposure increases the likelihood of developing a dependency later.
Emotionally, individuals experience a sense of novelty and euphoria, reinforcing continued use. Socially, initiation occurs in group settings, leading to a false sense of security about the risks involved. Financially, this stage has minimal impact, as use is infrequent. The long-term impact of addiction is not yet apparent, but early initiation is strongly correlated with a higher risk of later dependence. A study by the National Institute on Drug Abuse (NIDA) indicates that early drug use alters brain development, increasing susceptibility to addiction later in life.
2. Experimentation
Experimentation is marked by increased curiosity and voluntary engagement with a substance beyond the initial exposure. Individuals try different substances to assess their effects or use them in specific social contexts, such as parties. The frequency of use is still occasional but becomes more intentional rather than opportunistic. Behavioral changes include seeking out opportunities to use the substance, developing preferences for certain substances, and justifying use as harmless fun or stress relief.
Physically, mild but noticeable changes occur, such as increased tolerance or short-term side effects like nausea, dizziness, or altered cognitive function. Emotionally, individuals begin associating substance use with relaxation, pleasure, or escapism. Socially, users gravitate toward peers who also engage in substance use, which reinforces and normalizes the behavior.
Financially, there is minimal expenditure, but users start prioritizing substance-related activities. The impact of addiction is not yet fully realized, but patterns of experimentation set the stage for more frequent use. A study by Gray KM, Squeglia LM. et al. 2018, titled “Research Review: What have we learned about adolescent substance use?” suggests that individuals who experiment with substances in their teenage years have a significantly higher likelihood of developing substance use disorders later in life.
3. Regular Use
Regular use is characterized by a consistent pattern of substance consumption, though not necessarily daily. The individual begins integrating substance use into their routine, using it for stress relief, socialization, or coping with emotions. The frequency of use becomes more predictable, occurring on weekends, after work, or in specific situations. Behaviorally, users begin organizing their schedules around substance availability and experience cravings when they are unable to use.
Physically, early signs of dependence appear, such as withdrawal symptoms between uses or an increased need for higher doses to achieve the same effect. Emotionally, reliance on the substance for mood regulation.
In the United States, alcohol is the most commonly used and socially accepted substance. According to the National Survey on Drug Use and Health (NSDUH), approximately 85.6% of adults reported drinking alcohol at some point in their lifetime. However, about 14.5 million people aged 12 and older had an alcohol use disorder in 2020.
Illicit drug use is also prevalent. NSDUH data indicates that in 2020, 13.5% of individuals aged 12 or older reported using an illicit drug in the past month. Cannabis is the most commonly used illicit substance, with 17.9% of people aged 12 or older reporting use in the past year. The misuse of prescription drugs, particularly opioids, remains a significant concern. In 2020, 3.4% of individuals aged 12 or older misused prescription pain relievers.
Financially, spending on substances increases but remains within manageable limits. The impact of addiction starts manifesting subtly, as regular use increases the likelihood of developing compulsive behavior. Research from the Substance Abuse and Mental Health Services Administration highlights that regular use disrupts brain chemistry, particularly in the reward system, making the transition to dependence more likely.
4. Risky Use
Risky use represents a significant escalation in substance consumption, characterized by behaviors that pose dangers to the user and others. The frequency of use is higher, with individuals using substances despite experiencing negative consequences such as health issues, relationship conflicts, or declining performance at work or school. Behaviorally, users begin taking higher doses, mixing substances, or engaging in hazardous activities such as driving under the influence.
Physically, withdrawal symptoms become more pronounced, tolerance continues to increase, and the risk of overdose rises. Emotionally, mood swings, anxiety, and depression become more severe, leading to a cycle where the substance is used to alleviate these symptoms. Socially, conflicts with family and friends become frequent, and users isolate themselves or associate primarily with other substance users.
According to the National Survey on Drug Use and Health (NSDUH), about 21.5% of adults aged 18 and older reported binge drinking in the past month in 2022. Binge drinking is most prevalent among young adults aged 18 to 34, though it also affects older adults. Approximately 25% of high school students report engaging in binge drinking, increasing their risk for long-term health consequences.
Financially, the cost of sustaining use increases, leading to financial strain or risky behaviors such as borrowing money irresponsibly. The impact of addiction becomes more evident as daily life is increasingly centered around substance use. A study from the National Center for Biotechnology Information (NCBI) found that individuals in the risky use stage are at a significantly higher risk of transitioning into dependence, with brain imaging showing changes in impulse control and decision-making areas.
5. Dependence
Dependence is marked by a compulsive need to use a substance to function normally. The frequency of use is now daily or near-daily, with withdrawal symptoms occurring if use is stopped. Behaviorally, users prioritize substance use over responsibilities, experience unsuccessful attempts to cut down, and develop an increasing obsession with obtaining and using the substance.
Physically, significant changes occur, including chronic health problems, persistent withdrawal symptoms, and a weakened immune system. Emotionally, individuals experience heightened anxiety, depression, and mood instability, with an increasing inability to feel pleasure without the substance. Socially, relationships suffer as trust erodes and responsibilities are neglected.
Financially, addiction-related expenses lead to debt, job loss, or legal issues. The impact of addiction is profound, as dependence begins to dictate all aspects of life. According to a study by Goldstein RZ, Volkow ND. et al. 2011, titled “Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications,” prolonged substance dependence leads to alterations in the prefrontal cortex, impairing decision-making and impulse control.
6. Addiction
Addiction is the stage where substance use is no longer within the individual’s control. The frequency of use is compulsive and continuous, with individuals unable to abstain despite severe consequences. Behaviorally, addiction manifests as an inability to control cravings, engaging in risky activities to obtain substances, and experiencing severe cognitive impairments.
Physically, long-term damage occurs, including organ failure, brain deterioration, and increased mortality risk. Emotionally, individuals face extreme psychological distress, including paranoia, severe depression, and suicidal thoughts. Socially, most relationships are strained or severed, leading to isolation and legal troubles.
Financially, addiction leads to bankruptcy, homelessness, or criminal behavior to sustain substance use. The impact of addiction is life-altering, requiring professional intervention. A study by the World Health Organization (WHO) states that addiction is a chronic brain disorder rather than a moral failing, necessitating medical treatment and long-term recovery strategies.
7. Relapse
Relapse is the return to substance use after a period of abstinence, triggered by stress, environmental cues, or untreated psychological issues. The frequency of use varies, with some individuals experiencing a single lapse while others fall back into regular use. Behaviorally, relapse is marked by a loss of coping strategies, an overwhelming urge to use, and feelings of guilt or failure.
Physically, the risk of overdose is high due to reduced tolerance, and withdrawal symptoms return with intensity. Emotionally, individuals experience shame, frustration, and hopelessness, which perpetuate the relapse cycle. Socially, relationships suffer further, and support networks weaken.
Financially, relapse leads to additional losses, including employment and stability. The impact of addiction remains a persistent struggle, requiring renewed commitment to recovery. Research from the National Institute on Drug Abuse indicates that relapse rates for substance use disorders range from 40% to 60%, similar to other chronic diseases like hypertension, reinforcing the need for continued treatment and support.
Are the 7 Stages of Addiction the Same for All Substances?
No, the seven stages of addiction are not identical for all substances and behavioral addictions. While the general progression from initiation to addiction remains similar, the severity, duration, and impact of each stage vary depending on the substance or behavior involved. Highly addictive substances like opioids, methamphetamine, and nicotine lead to faster dependence and more intense withdrawal symptoms, making them harder to overcome. Alcohol and benzodiazepines also cause severe physical dependence, with withdrawal being potentially life-threatening.
In contrast, substances like marijuana or caffeine have milder withdrawal effects and a slower progression through the stages. Behavioral addictions, such as gambling, internet addiction, or compulsive shopping, follow a similar pattern to substance use disorders but primarily affect brain reward circuits rather than causing direct physical withdrawal. Overcoming addiction depends on factors such as the substance’s pharmacology, duration of use, genetic predisposition, and the availability of treatment and support systems.
What is Addiction?
Addiction is a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences. It involves functional changes to brain circuits involved in reward, stress, and self-control, leading to harmful behaviors.
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), addiction is classified under “Substance-Related and Addictive Disorders.” This category encompasses substance use disorders for various drugs and behavioral addictions like gambling disorder. The DSM-5 outlines criteria such as impaired control, social impairment, risky use, and pharmacological indicators (tolerance and withdrawal) to diagnose these disorders.
According to the National Survey on Drug Use and Health (NSDUH) conducted in 2021, approximately 20.4 million people aged 12 or older in the United States had a substance use disorder (SUD) in the past year. This includes 14.5 million individuals with alcohol use disorder and 8.1 million with illicit drug use disorder, highlighting the widespread impact of addiction nationwide.
What are the 4 C’s of the Cycle of Addiction?
The 4 C’s of the cycle of addiction are compulsion, control, craving, and consequences. These elements define the repetitive and self-destructive nature of addiction, where individuals struggle to break free from substance use despite recognizing its harmful effects. Each C plays an integral role in maintaining the cycle of addiction.
The 4 C’s of the cycle of addiction are as follows:
- Compulsion: Addiction begins with an overwhelming urge or compulsion to engage in substance use or a behavior. This compulsion is driven by changes in the brain’s reward system, making the individual feel an intense need to continue the behavior despite knowing the risks.
- Control: Over time, the ability to control substance use diminishes, leading to repeated consumption even in inappropriate situations. Individuals attempt to quit or cut back but are unable to do so, highlighting the loss of voluntary control over their actions.
- Craving: A strong psychological and physical craving develops as addiction progresses. These cravings arise from neurochemical imbalances in the brain, making individuals feel they need the substance to function normally. The intensity of cravings triggers relapse, even after periods of abstinence.
- Consequences: Despite experiencing negative effects on health, relationships, work, and finances, individuals continue using the substance. The consequences of addiction worsen over time, leading to legal problems, isolation, or severe health complications, reinforcing the destructive cycle.
What is the Difference between the Stages of Addiction and the Addiction Cycle?
The difference between the stages of addiction and the addiction cycle lies in their focus. The stages of addiction describe the progressive development of substance use disorder over time, from initiation to addiction and relapse, while the addiction cycle explains the recurring behavioral pattern that keeps individuals trapped in addiction.
The stages of addiction follow a linear progression, beginning with experimentation and leading to dependence and addiction. This model helps understand how substance use escalates and how early intervention prevents long-term addiction. In contrast, the addiction cycle is a repetitive pattern that individuals go through once addiction has taken hold, making it difficult to break free from compulsive substance use.
The addiction cycle begins with emotional triggers, such as stress, anxiety, or trauma, that create psychological distress. These emotions lead to cravings, an intense urge to use the substance as a way to cope. Cravings then progress into a ritual, where individuals engage in predictable behaviors leading up to substance use, such as visiting certain places or interacting with specific people associated with their addiction.
Once the ritual is complete, the individual engages in substance use, experiencing temporary relief or pleasure. However, after the effects wear off, guilt sets in. This stage is marked by shame and regret, which further reinforce emotional distress, restarting the cycle. Unlike the linear nature of the stages of addiction, this cycle is ongoing and self-perpetuating, making recovery challenging without intervention.
It is important to understand both models of treatment, as breaking the addiction cycle requires addressing emotional triggers and cravings, while preventing addiction requires early recognition of the stages leading to dependence.
Do Behavioral Addictions Have the Same Stages?
Yes, behavioral addictions follow similar stages as substance addictions, but with some differences in physical dependence and withdrawal symptoms. Both types progress from initial engagement to compulsive behavior, but behavioral addictions primarily affect brain reward circuits rather than causing direct chemical dependency.
The stages of behavioral addiction begin with initiation, where an individual is first exposed to an activity such as gambling, gaming, or social media use. Experimentation follows, where the behavior is occasionally engaged as a form of entertainment. Regular use develops when the activity becomes a habitual coping mechanism. Risky use emerges when the behavior starts interfering with daily responsibilities, leading to negative consequences. Dependence is marked by an inability to stop despite adverse effects, followed by addiction, where the individual loses control over their actions. Relapse occurs when individuals attempting to quit return to compulsive behavior like substance use, triggered by stress or environmental cues.
How Is Addiction Diagnosed?
Addiction is diagnosed using clinical criteria that assess behavioral patterns and impairment. The DSM-5 classifies substance use disorders and behavioral addictions under “Substance-Related and Addictive Disorders.” Diagnosis requires meeting at least two of 11 criteria, including loss of control, increased tolerance, withdrawal symptoms, persistent cravings, and continued use despite negative consequences.
Mental health professionals use structured interviews, self-report assessments, and behavioral observations to determine the severity of addiction. More symptoms indicate a more severe disorder, which helps guide treatment decisions. Addiction is recognized as a chronic condition requiring long-term intervention strategies, including therapy, medication, and behavioral modifications.
What Treatments are Available at the Different Stages of Addiction?
The treatments available at the different stages of addiction are detox, medication-assisted treatment (MAT), behavioral therapies, and support groups. Each treatment is designed to address specific stages of addiction, from early dependence to long-term recovery, and their effectiveness varies based on the type and severity of the addiction.
The following treatments are available at the different stages of addiction:
- Detox: Detox is the first step in treating substance dependence and is most effective during the transition from regular use to risky use or dependence. Detoxification helps remove toxic substances from the body and manage withdrawal symptoms under medical supervision. According to WebMD, detox is paramount for addictions to alcohol, opioids, and benzodiazepines, where withdrawal is severe or life-threatening.
- Medication-Assisted Treatment (MAT): MAT is used primarily for opioid and alcohol addiction in the dependence and addiction stages. MAT combines FDA-approved medications like methadone, buprenorphine, or naltrexone with counseling to reduce cravings and prevent relapse. Research by Bahrami K, Kuo YF, Digbeu B, Raji MA. et al. 2023, titled “Association of Medication-Assisted Therapy and Risk of Drug Overdose-Related Hospitalization or Emergency Room Visits in Patients With Opioid Use Disorder,” shows that MAT significantly improves treatment retention and reduces overdose risks by more than 50%.
- Behavioral Therapies: Behavioral therapies are important at all stages of addiction, especially during risky use, dependence, and recovery. Therapies like Cognitive Behavioral Therapy (CBT) and Contingency Management (CM) help individuals change their thought patterns, develop coping strategies, and modify behaviors that contribute to addiction. These therapies are effective for both substance use and behavioral addictions, such as gambling or internet addiction. According to Verywell Mind, around 60% of individuals treated with CBT for addiction maintain their recovery for a year, and CBT reduces substance use in a significant portion of participants.
- Support Groups such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) play an integral role in long-term recovery and relapse prevention. These groups provide peer support, accountability, and a sense of community. They are particularly effective after initial treatment phases, helping individuals maintain sobriety and navigate triggers that lead to relapse. Research by the CDC shows that up to 90% of people who receive this type of addiction support are less likely to use drugs after two years than those who don’t.
What are the Stages of Change in Addiction Recovery?
The stages of change in addiction recovery are Precontemplation, Contemplation, Preparation, Action, and Maintenance. These stages of change represent the psychological and behavioral shifts individuals go through when overcoming addiction, helping to guide treatment approaches based on their readiness for change.
The following are the stages of change:
- Precontemplation: Precontemplation is the stage where individuals are not yet aware of their addiction or deny its severity. They resist change and rationalize their substance use. At this stage, external interventions such as education and motivational interviewing are necessary to help them recognize the need for recovery.
- Contemplation: Contemplation occurs when individuals acknowledge their addiction but feel ambivalent about change. They begin weighing the pros and cons of quitting but lack commitment. Counseling and self-reflection exercises are useful in strengthening their motivation to move forward.
- Preparation: Preparation is when individuals actively plan to change and take small steps toward recovery, such as seeking information about treatment or reducing substance use. This stage is important for setting goals and establishing a support system, which increases the likelihood of successful long-term recovery.
- Action: Action is when individuals make significant lifestyle changes, such as entering a treatment program, practicing sobriety, or attending therapy. This is a necessary phase where commitment is tested, and structured interventions like detox, behavioral therapy, and support groups provide important guidance.
- Maintenance: Maintenance focuses on sustaining recovery and preventing relapse. Individuals in this stage develop coping mechanisms, avoid triggers, and maintain healthy habits. Long-term engagement in therapy, peer support, and self-care practices is important to ensuring lasting recovery and preventing setbacks.
How Does Treatment Differ Depending on the Stage of Addiction?
Treatment differs depending on the stage of addiction, as early-stage interventions focus on education and behavioral therapy, while advanced stages require intensive medical and psychological support. The severity of addiction determines whether an individual needs outpatient counseling, intensive outpatient programs (IOP), partial hospitalization programs (PHP), or inpatient rehabilitation.
In the early stages, such as experimentation or regular use, outpatient treatment, including individual therapy and group counseling, is effective in preventing progression. Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI) are commonly used to address risky behaviors and strengthen coping skills.
As addiction progresses to risky use or dependence, more structured programs like Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP) become necessary. These programs provide a higher level of care, including medical monitoring and structured therapy, while allowing individuals to maintain some daily responsibilities.
For severe addiction, especially in the dependence and addiction stages, inpatient rehabilitation is required. Residential treatment centers offer 24/7 medical supervision, detox, and intensive therapy to manage withdrawal symptoms and address deep-rooted psychological issues. Medically assisted detox is also necessary for substances like alcohol or opioids.
In the recovery and relapse stages, ongoing aftercare, such as 12-step programs, sober living homes, and continued outpatient therapy, helps individuals maintain long-term sobriety. The right treatment approach depends on the individual’s level of addiction, co-occurring mental health disorders, and personal circumstances.
How to Prevent the Relapse Stage?
To prevent the relapse stage, individuals must adopt long-term strategies such as therapy, medication management, lifestyle changes, and strong support systems. Relapse prevention techniques include identifying triggers, developing coping mechanisms, and engaging in ongoing treatment programs like relapse prevention programs and aftercare. A study by McKay JR. et al. 2021, titled “Impact of Continuing Care on Recovery From Substance Use Disorder,” indicates that structured aftercare programs significantly reduce relapse rates.
Can You Skip a Stage of Addiction?
Yes, you can skip a stage of addiction, though it is uncommon. Some individuals transition rapidly from experimentation to dependence due to genetic predisposition, mental health conditions, or the potency of the substance used, as studied by Wang JC, Kapoor M, Goate AM. et al. 2012, titled “The genetics of substance dependence.” Research from the National Institute on Drug Abuse (NIDA) highlights that highly addictive substances like fentanyl lead to rapid dependency, bypassing the early stages.
How Long Does It Take to Progress Through the Stages of Addiction?
It takes months or even years to progress through the stages of addiction, depending on factors such as substance type, frequency of use, genetic vulnerability, and mental health status. Some individuals develop an addiction within weeks, while others take years. According to NIDA, in “Understanding Drug Use and Addiction DrugFacts,” the progression is accelerated by early exposure, high-potency substances, and repeated use.
Opioids, particularly fentanyl, are among the fastest and most addictive drugs, as studied by NIDA, causing dependence within days of regular use. Fentanyl is 50 times more potent than heroin, leading to a high risk of overdose. Alcohol addiction, in contrast, develops more gradually over months or years, though binge drinking accelerates dependence. Stimulants like methamphetamine and cocaine also have a high addiction potential but take longer than opioids. Marijuana and benzodiazepines tend to develop dependence over prolonged use, though withdrawal symptoms are still severe.
At What Stage Does Addiction Become a Chronic Disease?
At the dependence stage, addiction becomes a chronic disease as the brain’s reward system undergoes lasting changes. The American Society of Addiction Medicine (ASAM) states that dependence leads to compulsive substance use, making addiction a chronic condition requiring long-term management, similar to other chronic illnesses like diabetes or hypertension.
In the United States, chronic diseases like diabetes and hypertension affect a significant portion of the population. These diseases can be caused by long term drug and alcohol abuse. According to the National Diabetes Statistics Report, approximately 38.4 million people of all ages, or 11.6% of the U.S. population, had diabetes in 2021. Similarly, hypertension, or high blood pressure, is prevalent among U.S. adults, with nearly half (47%, or 116 million) diagnosed with this condition. Both diseases pose substantial public health challenges, necessitating ongoing prevention, management, and treatment efforts.
What Are Common Relapse Triggers at Different Stages of Addiction?
Common relapse triggers at different stages of addiction are stress, environmental cues, emotional distress, and social influences. In early recovery, withdrawal symptoms and cravings are major triggers, while in long-term recovery, complacency and overconfidence lead to relapse. Research from the Journal of Substance Abuse Treatment shows that emotional distress is one of the strongest predictors of relapse.
How Do Mental Health Disorders Impact the Progression of Addiction?
Mental health disorders impact the progression of addiction by increasing vulnerability to substance abuse and making treatment more complex. Conditions like anxiety, depression, and PTSD drive individuals to self-medicate, accelerating addiction. The National Institute of Mental Health (NIMH) reports that nearly 50% of individuals with addiction also have a co-occurring mental disorder, which worsens substance dependence. A study by Sinha R. et al. 2008, titled “Chronic stress, drug use, and vulnerability to addiction,” Stress pathways increase cravings, weaken self-control, and drive compulsive substance use, leading from casual use to chronic addiction despite negative consequences.
Can Addiction Treatment Be Effective at Any Stage?
Yes, addiction treatment can be effective at any stage, but earlier intervention leads to better outcomes. Evidence-based treatments, including medication-assisted therapy (MAT) and behavioral counseling, help individuals regain control, even in severe addiction cases. A study by McKay JR. et al. 2021, titled “Impact of Continuing Care on Recovery From Substance Use Disorder,” confirms that long-term treatment engagement significantly improves recovery success, regardless of addiction severity.




 FindTreatment.gov
FindTreatment.gov